CHAPTER I
INTRODUCTION
1.1 Background
Cardiac Pulmonary Resuscitation is very important in the life of the medical world, so that every doctor should be able to perform Cardiac Pulmonary Resuscitation. Well as other paramedics. In fact, any layperson who works in a place where a lot of people (the crowd) or the place where a lot of work to contain the risk of work should be able to be trained in Cardiac Pulmonary Resuscitation is a simple to a more competent medical officer. B-gels or in the Indonesian language known as the Emergency First Aid (PPGD) is the set of the first attempts to do in emergency conditions in order to save patients from death. Abroad, PPGD is actually taught in many ordinary people or ordinary people special, but it seems this is still very little known by the people of Indonesia.
1.2 Key Principles
PPGD is the main principle of saving the patient from death in emergency conditions. Later in the PPGD philosophy is "Saving Time is Life Saving", in the sense that all actions taken during emergency conditions to be truly effective and efficient, because the patient's condition may have lost their lives in just minutes (stopping breathing for 2 -3 minutes can cause death).
1.3 Basic Steps
The basic steps in PPGD known by the acronym ABCD (Airway - Breathing - Circulation - Disability). These four points are the points that should be kept in the response of patients in emergency conditions.
1.4 Pulmonary Resuscitation heart
Stop the breath because:
- Airway Obstruction
- Foreign bodies
- Aspiration
- The tongue falls down
- Pipe folded endotracheal
- Blocked tracheal cannula
- Acute Abnormalities of the glottis and surrounding
- Depression of central respiratory
- Drugs
- Intoxication
- High pCO2
- Low pO 2
- After the cardiac arrest
- Brain tumors
- Sunset
Peripheral:
- Drug muscle paralytic
- Myasthenia gravis
- Poliomyelitis
For the Stop Heart
1. Cardiovascular (heart disease siskemik, IMA, pulmonary embolism and conduction system fibrosis)
2. Acute oxygen deficiency (stopping breathing, and obstruction due to foreign body secretions)
3. Overdose of drugs (digitalis and adrenaline)
4. Acid-base disturbances / electrolyte (K increases or decreases, increased Mg, Ca increases, acidosis)
5. Accidents (electric shock, drowning)
6. Vagal reflex
7. Anesthesia and surgery
8. Medical diagnostic and therapeutic measures
9. Shock, cardiac arrest can be accompanied by electrical phenomena.
Adam Stokes syndrome
Condition caused by high degree AV block heart is characterized by episodic bradycardia or asystole that resulted in the attack who are not aware of themselves suddenly with / without a seizure action.
- Artificial Circulation
- External cardiac massage
Indications CPR: Stop or stopping breathing and circulation.
Contraindications: Cardiac arrest, rib fractures, thoracic fractures, cardiac tamponade, pneumothorax, severe emphysema, Cardiac Arrest over 5-6 minutes.
1.5 Identify critical patient and / or patients who are not aware
To recognize all the things that threaten the lives and doing therapy right away, we should be able to immediately identify critical patient quickly and simply. In many cases, the cause of this patient's condition is unclear, but may be helpful to remember ABCBA:
A: Airway (airway)
B: Breathing (Respiratory)
C: Circulation (Circulation)
D: Defribilation (electrical therapy)
The first assessment only takes a few moments:
A: Check if the patient's airway
B: Check whether the patient is breathing, if not then needed artificial respiration
C: Check the pulsation of the arteries (carotid a. / a. Femoral), if there is failure of circulation, begin to perform external cardiac massage immediately.
D: Assess whether the patient suffered cardiac arrest or heart rhythm disturbances, if there is then given electric therapy
CHAPTER II
DISCUSSION
2.1 Definitions
As the measures taken to relieve the airway while maintaining cervical control.
2.2 Objectives
Resuscitation is an action that must be performed immediately in an effort to save lives (Hudak and Gallo, 1997). Resuscitation was initiated with the appropriate assessment of patient awareness kradaan and then continue with the provision of basic life support (Basic life support) aimed at emergency oxygenation. (AHA, 2003).
Purpose of phase II (Advance life support) is to restart spontaneous circulation, whereas the purpose of phase III (prolonged life support) is a post-resuscitation intensive pengelolahan, the final results of resuscitation will depend on the speed and accuracy penolongpada first phase in providing life support basis.
The main purpose of protecting the brain resuscitation kardiopulmonar manually from lack of oxygen, there is better blood circulation, although the black than nothing. Circulation to ensure adequate oxygenation is needed immediately because the cells - brain cells become paralyzed when the oxygen to the brain stops for 8-20 seconds and will die if the oxygen suspended for 3-5 minutes (Tjokronegoro, 1998). Damage in the form of disability or even death.
CPR Phase 2.3
The division of this phase is intended to facilitate the training and recall phase needs to be done. Noteworthy is also the readiness of rescue, whether capable or not and the environment, whether or not to alienate the patient or the patient in a dangerous environment.
a. Phase I: Basic Life Support (BLS), the emergency rescue procedures in dealing with airway obstruction, cardiac arrest and how to perform CPR correctly. In this phase consists of steps in A (airway), B (breathing), C (circulation).
- A (Airway): Keeping the airway open
- B (Breathing): pulmonary ventilation and adequate oxygenation
- C (Circulation): Hold the circulation by compression of the artificial heart lung
b. Phase II: Advance Life Support (ALS), the BLS added to D (drug) and E (EKG).
- D (drugs): Delivery of medicines including liquid.
- E (EKG): Diagnosis elektrokardiografis know as soon as possible to ventricular fibrillation.
c. Phase III: prolonged Life Support (PLS), namely the addition of BLS and ALS, G (gauge), H (head), I (Intensive care).
- G (Gauge): Measurement and inspection for continuous monitoring of patients, assessed, looking for the cause and then treat it.
- H (Head): Pindakan resuscitation to save the brain and nervous system from further damage due to cardiac arrest, so as to prevent the occurrence of permanent neurologic.
- I (Intensive Care): Intensive Care in the ICU, namely: tracheostomy, continuous controlled breathing, stomach sonde, measuring pH, pCO2 and support when needed if seizures mengedalikan circulation.
Before performing the steps A (airway) first performed the initial procedure in patients / victims, namely:
- Ensuring environmental safety.
Safe for the rescuers and safe for patients / victims themselves.
- Ensure awareness of patient / victim.
In ensuring patient / victim can be done by touching or shaking the shoulders of the patient / victim with a soft and steady, while calling his name or sir! / Mom! / Mas! / Ma'am!, Etc..
- Ask for help
When it is believed the patient / victim is unconscious or there is no immediate response to call for help by the way: yelling "help!" Let the position where, use existing communication tools, or activate the bell / emergency systems in place (in a hospital emergency bell) .
- Improving the patient / victim.
BHD action is effective when the patient / victim in a supine position, located on a flat surface / hard and dry. If found the patient / victim side or face down on the patient / victim should be stretched first in reverse as a unified whole to prevent injuries / complications.
- Adjust the position of helper.
Helper kneeling position with your shoulders parallel to the patient / victim to the rocks while giving rescue breathing and circulation assistance do not need a lot of movement.
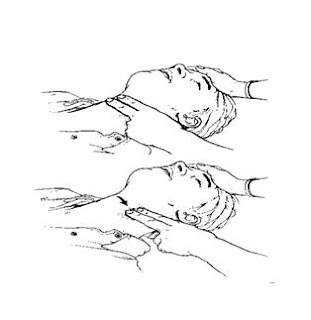
Figure 1.
Check the Enable awareness and Emergency Systems
A. A: (Airway) Street Breath
1. Road checks Breath
To ensure free airway obstruction due to foreign objects. When there are blockages can be cleared with the technique of cross finger (the thumb with the index finger is placed opposite the mouth of the victim).
How to perform a cross finger technique
a. Cross your thumb and forefinger helper
b. Put your thumb on the lower incisors victim / patient and forefinger on the upper incisors
c. Do it like a cutting motion to open the mouth of the patient / victim.
d. Check the mouth after open if there is fluid, foreign bodies that obstruct the airway.
2. Making Way Breath
In the patient / victim is not aware of muscle tone disappeared, the tongue and epiglottis to close the pharynx and larynx causing airway obstruction. This situation can be released with prop head tilted forehead (Head tild Chin lift) and maneuvering pushing the mandible (Jaw thrush maneuver).
How to perform a head tilt chin lift technique.
a. Put your hand on the forehead of the patient / victim
b. Press forehead slightly forward with your palms helper
c. Put your other fingers below the tip of the jaw bone of patients / casualties
d. Tilt of the head and hold / press the forehead of patients / victims heads together until the patient / victim to the position of the extension.
How to perform a jaw thrust maneuver techniques
a. Put your elbows parallel to the position of the patient helper / victim
b. Both hands holding the sides of the head of the patient / victim
c. Helper to hold both sides of the jaw
d. Second hand helper to move the jaw forward position slowly
e. Maintain the position of the mouth of the patient / victim remains open
Figure 2. Liberation Road Breath Head tilt chin lift technique (a)
and jaw thrust maneuver technique (b)
(a) (b)
2. B: (Breathing) Help Breathing
The principle is to provide two times the compression and ventilation before giving vent 2 times per 10 seconds on the time after compression. Consists of two stages:
A. Ensure the patient / victim is not breathing
By:
- Look: Check whether there is movement of the chest (breathing motion), whether the motion is symmetrical?
hear the breath sounds (listen) Listen if there is a normal breath sounds, and whether there are additional abnormal breath sounds (because there are no obstacles could arise in part).
- Feel: Feel the cheek examiner if there is breathing air from the victim?
If the patient was still breathing, then calculate how much the patient's respiratory rate in 1 minute (normal breathing is 12 -20 times per minute).
The types of additional breath sounds airway obstructions in part:
a. Snoring: snoring sounds like, this condition indicates the existence of a deadlock the upper airway by a solid object, if the sound of this then do check directly by cross-finger to open the mouth (using two fingers, the thumb and index finger are used to chin lift before, pushing your thumb into the upper jaw, lower jaw index finger pressed down). See if there is a related object in the throat of victims (eg: false teeth, etc.). Move the object
Figure 3 Cross Finger

b. Gargling: sounds like gargling, this condition occurs because there is a deadlock caused by the fluid (eg: blood), then do a cross-finger (as above), then do the finger-sweep (as the name implies, use two fingers are wrapped with a cloth to "sweep" of the oral fluids).
Figure 4 Finger Sweep

c. Crowing: high-pitched voice, usually be caused due to swelling (edema) in the trachea, to keep doing the first aid maneuvers head tilt and chin lift or jaw thrust alone.
If breath sounds are not heard because there are a total resistance of the airways, it can be done:
Blow a.Back 5 times, namely by using the palm of the hand hitting the area between the scapula bone in the back
b.Heimlich Maneuver, by positioning itself as a picture, then pulled back toward the upper hand.
Figure 5. Heimlich Maneuver

c.Chest Thrust, performed on pregnant women, infants or obese by positioning itself as an image and push the hand towards the top.
Figure 6. Chest Thrust

Listen:
- If normal breathing frequency, monitor the patient's condition continued to keep doing the Look Listen and Feel.
- If the frequency of breath <12-20 beats per minute, give breathing assistance (breathing assistance detailed below)
- If the patient has stopped breathing give artificial respiration (artificial breathing detailed below)
Having given artificial respiration then do permeriksaan carotid arteries located in the neck (check with two fingers, put your finger on the bulge in the middle of the throat, then move your finger to the side, until inhibited by the neck muscles (Sternocleidomastoideus), feel the carotid pulse for 10 seconds.
Figure 7. Check breathing
Checking the carotid pulse
- If there is no pulse then do heart massage (figure D and E, figure F in infants), followed by artificial respiration (figure A, B and C), repeated up to 6 times the cycle of cardiac massage, artificial breathing, which ends with a massage the heart.
Figure 8

Heart massage (figure D and E, figure F in infants), followed by artificial respiration (figure A, B and C).
- Check the carotid pulse again (with the method as above) for 10 seconds, if palpable do Look Listen and Feel (back to point 11) again. if not palpable repeat point number 17.
- Heart massage and artificial respiration was stopped if
a. Helper fatigue and had no more power
b. Patient already showing signs of death (rigid bodies)
c. Help been dating
d. Palpable carotid pulse
- After successfully securing the above conditions check the signs of shock in patients:
a. Beat rate> 100 beats per minute
b. The palm wet hands cold and pale
c.Capilarry Refill Time> 2 seconds (CRT can be checked by pressing the tip of the nail polish dg patients examiner for 5 seconds, then release, which checks how long it takes for the red color of the nails again)
- If the patient is in shock, do the Shock Position in patients, ie patients with a raised leg as high as 45 degrees in the hope it would be a lot of blood circulation to the heart
Figure 9, Shock Position
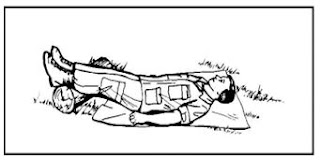
- Maintain the position of shock until help arrives or signs of shock disappears
- If there is bleeding in patients, is trying to stop the bleeding by pressing or bandage the wound (do not bandage too tightly as it can lead to tissue death bandaged reply)
- After the patient's condition is stable, remains always monitor the condition of patients with Look Listen and Feel, because patients sometimes can deteriorate suddenly.
Breath Help
Assistance breath is the breath that is given to patients to normalize the patient's breathing frequency is below normal. Eg respiratory rate: 6 times per minute, then it should be given breath in between each breath help him so that the total spontaneous breathing permenitnya be normal (12 times).
A. Provide breathing assistance
Help the breath can be done through word of mouth, mouth to nose, mouth to stoma (a hole made in the throat). Respiratory assistance given by 2 times, each time blowing time from 1.5 to 2 seconds and the volume of 700 ml - 1000 ml (10 ml / kg or until visible chest patients / victims expands. Given oxygen concentration 16-17%. Note the patient's response .
The procedure is:
1. Position yourself next to the patient
2. Do not perform mouth to mouth breathing immediately, but was using fabric as a barrier between you and the patient's mouth to prevent the transmission of the disease - the disease.
3. While doing chin lift, use the hand that had been used for head tilt to cover the patient's nose (so do not waste air given through the nose).
4. Eyes are watching the patient's chest
5. Cover the entire mouth to mouth rescue victims
i. Word of mouth
Is a fast and effective. At the time of giving mouth rescue breathing and rescue cover all the patient's mouth / nose victims and the patient / victim should be closed with the forefinger and thumb helper. Volume of air that can cause excessive air into the stomach.
Figure 10. Giving breath of mouth

Recommended if assistance from the victim's mouth is not possible, such as patient / victim had trismus or severe injuries. Helper should close the mouth of the patient / victim at the time of giving aid breathing.
Figure 11. From mouth to nose breathing

Performed on the patient / victim is installed or run laringotomi tracheostomy.
Figure 12. Mouth-to-stoma breathing.

Cardiac massage procedures:
1. Position yourself next to the patient
2. Position the hands as shown in the center of the chest (right in the middle of the chest)
Figure 13. Hand position on the patient's chest

Figure 14. hand upright position

4. Press victim's chest using power obtained from the hip joint (hip joint)
5. Press chest approximately 4-5 cm depth (as shown below left)
Figure 15. how to compress the chest

7. A set of cardiac massage performed some 30 times the pressure, to facilitate the count can be calculated by calculating the following:
One Two Three Four ONE
One Two Three Four Two
One Two Three Four Three
One Two Three Four Four
One Two Three Four Five
One Two Three Four Six
8. Cardiac massage principles are:
a. Push deep
b. Push hard
c. Push fast
d. Maximum recoil (cardiac relaxation time given)
e. Minimum interruption (at the time of this procedure should not be interrupted helper).
4. D: (DEFIBRILATION) electrical therapy
Therapy performed by delivering electrical energy to the patient / victim which causes cardiac arrest is a heart rhythm disorder. The main cause is ventricular tachycardia or ventricular fibrillation. On the use of lay people available AED.
Assessor re:
After 4 cycles of compression and ventilation and the patient / victim re-evaluated:
i. If no heart rate do compression and breathing assistance with a ratio 30: 2
ii. If there is breathing and heart beat palpable put the victim in the position of the steady
iii. If there is no breath but palpable heart rate, breathing give assistance as much as 12 times per minute and heart rate monitor at all times.
2.4. Self Protection Helper
In conducting the rescue in an emergency condition, rescuers still have to constantly ensure the safety of himself, both from the dangers caused by the environment, and because of the danger caused by the provision of aid.
2.5 The key points in the protection of self-helpers:
1. Make sure the conditions of succor and relief will not harm the patient
2. Minimize direct contact with patients, which is why in providing assistance wherever possible to use breath handkerchief or other cloth to protect rescuers from diseases that may be transmitted by the victim
3. Always look at the health self-rescuers, for the provision of first aid is the act of a very energy consuming. If done with a condition not fit, it will endanger the rescuers themselves.
2.6 Guidelines for Cardiac Pulmonary Resuscitation Latest Update 2010
American Heart Association (AHA) recently published guidelines for cardio pulmonary resuscitation and emergency cardiovascular care 2010. As we all know, scientists and health practitioners continue to mengeavaluasi CPR or the more we are familiar with CPR and published every 5 years. Conducted a thorough evaluation of the order and priority includes the steps of CPR and adapted to today's scientific advances fatherly identify factors that have the greatest impact on survival. On the basis of the strength of available evidence, they develop a recommendation to support interventions that demonstrate the most promising results.
Recommendations in the 2010 Guidelines confirm the safety and effectiveness of many approaches, acknowledge ineffectiveness of others and introducing new treatments based on an intensive evaluation of evidence and consensus of experts. The presence of this new recommendation is not to suggest that earlier guidelines is unsafe or ineffective.
After evaluating a variety of studies have been published over the last five years the AHA Cardiac Pulmonary Resuscitation Guidelines issued (CPR) 2010. 2010 was the main focus is the quality of CPR chest compressions. Here are some differences between the CPR 2005 CPR guidelines 2010. Not anymore but ABC CAB Earlier in the first aid guidelines, we know the ABC: Airway, Breathing and Chest compressions, which is open airway, assisted respiration and chest compression. Current chest compression first, then we can focus on the airway and breathing. The only exception is only for the newborn. However, for infant CPR, child CPR, or CPR adult, should receive chest compressions before we think of providing airway.
1. No more looking, listening and feeling
The main key to save a person with cardiac arrest is the act, not a judge. Call an ambulance right away when we see the victim is conscious and do not breathe properly. Believe in your guts, if you try to assess the victim is not breathing or with your cheek close to the mouth of the victim, it is fine. But still, the victim is not breathing and the action look, feel, listen this is only going to spend time
2. Chest compressions deeper.
How deep you have to press the chest CPR has changed in 2011. Previously, he was 1 ½ to 2 inches (4-5 cm), but the AHA now recommends for pressing at least 2 inches (5 cm) on the chest.
3. Chest compression even faster.
AHA replace the editorial line here. Previously written: chest press about 100 compression per minute. AHA now recommends us to compress the chest at least 100 compression per minute. At this speed, 30 compression takes 18 seconds.
4. Hands only CPR
There are differences in technique from that of 2005, but the AHA CPR encourages this kind in 2008. AHA still wants the untrained rescuers perform CPR on Hands only adult victims who collapse in front of them. The big question is: what should be done untrained rescuers to the victims who did not pass out in front of them and the victims are not an adult / AHA does not give an answer on this but here there is a simple suggestion: provide hands-only CPR for doing something is better not daripda do at all.
5. Recognize sudden cardiac arrest
CPR is the only governance for sudden cardiac arrest and the AHA asks us alert and perform CPR when it happened.
6. Do not stop pressing.
Any cessation of chest compressions means to stop the blood to the brain resulting in the death of brain tissue when blood flow stopped for too long. Requires some chest compression to draw blood again. AHA wants us to continue to push as long as we can. Continue to press until the automatic defibrillator devices come in and be ready to assess the state of the heart. If it is time for breathing from mouth to mouth, do it soon and get back on pressing the chest.
Airway Management 2.7 (Maintenance of the airway) with Tool
How this is done if the airway management without the tool does not work perfectly and the facilities available.
Equipment can be:
a. Installation of Pipe (tube)
• Installed artificial airway with a pipe, a pipe can oropharynx (mayo), nasopharyngeal or endotracheal tube pipe depending on the condition of the victim.
• The use of pipe can be used to maintain the oropharyngeal airway remains open and hold the base of the tongue from falling back to close the airway, especially for people with no conscious
• Installation of the endotracheal tube will ensure the airway remains open, to avoid aspiration and facilitate breathing assistance measures
b. Liquid suction (suctioning)
• If there is a blockage of the airway liquid. Performed with the suction tool of suckers (sucker manually or by machine)
• In patients with trauma to the basis cranii is hard to use suction to prevent the suction into the base of the skull
c. Cleaning of solid foreign bodies in the airway
• If the patient does not realize there is a blockage of solids in the hypopharynx is not possible to do a sweep of a finger, then use a tool such as: laryngoscope, a vacuum and forceps.
d. Opening the airway
• Can be done krikotirotomi or tracheostomy
• This method is chosen when the cases where the installation of an endotracheal tube is not possible, the selected action krikotirotomi with a needle. For trained medical personnel, can do krikotirotomi with a knife or a tracheostomy.
e. Protection of the cervical
• In managing the airway, not to forget the cervical control, especially in multiple trauma or suspected cervical spine injury.
• Installed from the scene. Keep the neck do not move much. The position of the head should be "in line" (in line with the vertical axis of the body)
2.8 Specific Helper to provide CPR
A. Untrained rescuers (Untrained lay rescuer)
for the layman who is not experienced only chest compressions performed.
2. Helpers who are trained (Trained lay rescuer)
Should give chest compressions to the patient SCA (sudden cardiac arrest) and may provide ventilation to the ratio 30: 2.
3. Health care providers (Healthcare Provider)
Resuscitation are given depending on the case at hand. If there are patients who are weak or who have airway obstruction and decreased awareness, CPR can also be provided with chest compressions 30 times and passed on to the vent. If you find a patient who is unresponsive or not breathing, the assumption of SCA (Sudden Cardiac Arrest) has always done.
2.9 CPR in special circumstances
1. Sink
Drowning is the leading cause of preventable death. Success depends on helping the victims drowned long and weigh the degree of hypoxia.
Figure 20. CPR on a drowning victim

2. Hypothermia
In the unconscious patient because of hypothermia, rescue breathing should be assessed to determine whether there is stopping breathing and pulse rate under on assessing the presence or absence of a cardiac arrest or bradycardia for 30-45 seconds because heart rate and breathing very slowly depending on the degree of hypothermia.
If the victim is not breathing, give artificial respiration immediately. If no pulse do chest compressions immediately. Do not wait for a warm body temperature. To prevent the loss of the victim's body heat, remove wet clothing, put a warm blanket if possible give a warm oxygen.
2:10 The position of the solid (Recovery Position)
This position is used for an unconscious victim who had normal breathing and circulation is safe. This position was created to keep the airway open and reduce the risk of airway obstruction and aspiration. The way the victim is placed tilted on one side of the body with hands in front of the body below.
CHAPTER III
CONCLUSION
2. To assess airway examination, there are three stages, namely:
* L = Look / See the movement of breath or chest development, the retraction between the ribs, the color of the mucosa / skin and awareness
* L = Listen / Listen respiratory airflow
* F = Feel / Feel the presence of respiratory air flow by using a cheek helper
3. Compression is done first in case there is a stop or stop breathing
heart because every second that do not harm the compression of the blood circulation and reduce the number of victims safety.
4. The procedure is the latest CPR chest compressions 30 times with 2 breaths made.
REFERENCE
1. Dobson, Michael B; alih bahasa, Adji Dharma. 1994. Penuntun Praktis Anestesi (at the district hospital ). Penerbit buku kedokteran EGC. Jakarta.2. Latief S.A. 2007. Petunjuk Praktis Anestesiologi. Edisi Kedua. Penerbit FKUI. Jakarta.
3. Overview of basic life support in infants and children. Diakses dari http://www.uptodate.com/patients/content/topic.do?topicKey=~ZZjtriYsdaYe/.
4. Bantuan Hidup Dasar. Diakses dari http://www.scribd.com/doc/4535323/bantuan-hidup-dasar.
5. http://www.scribd.com/doc/45828899/Airway-Management-Kgd
6. http://akatsuki-ners.blogspot.com/2010/12/pertolongan-pertama-pada-gawat-darurat.html


No comments:
Post a Comment