CHAPTER II
Fistula ANI
I. DEFINITION
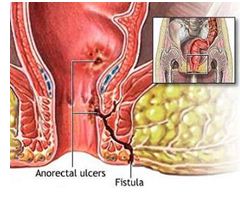
Fistula ani also called perianal fistula or fistula para-anal1. Anorectal Fistula (Fistula ani) is an abnormal communication between the anus and perianal skin. Glands in the canal lies in linea dentate ani provides a pathway for the infecting organism can achieve intramuscular2 space.
II. Etiology
Fistulas can occur spontaneously or secondary to perianal abscess (or perirektal). In fact, after drainage of the abscess periani, nearly 50% are likely to develop into a chronic fistula. Other fistulas may occur secondary to trauma, Crohn's disease. ani fissures, carcinoma, radiation therapy, aktinomikosis, tuberculosis, and infections klamidia2.
Kriptoglandular hypothesis states that an infection begins in the gland ani and evolve into the muscular wall of the anal sphincter causing anorectal abscess. After surgical or spontaneous drainage periani on the skin, usually of the granulation tissue tract behind, causing symptoms berulang2.
Can be caused by perforation or abscess penyaliran anorektum. Sometimes fistula caused by colitis with proctitis, such as tuberculosis, amubiasis, or morbus Crohn. Infection of the anal glands intersphincter in organisms found in the gastrointestinal tract-either aerobic (Cth: E. coli) and anaerobes (Cth: Bacteroides spp.) - Is a common disorder that causes ini.1
III. ABSCESS ANOREKTUM
Perianal abscess usually occurs due to an infected gland analyst eroded into the underlying tissues. Cultures from the rectum anal fistula abscess showed mixed infection with E.coli dominant. Chronic use of regionalist purgatif and enteritis is a common factor. Unusual infections such as aktinomikosis, tuberculosis, and other fungal diseases, pelvic inflammatory disease, prostatitis and cancer can rarely menyertai3.
Early symptoms of dull pain in the rectum and mild systemic complaints perianal pain continues to be severe throbbing with fever, chills, and malaise. Regional fluctuations are not always clear, because perianus thick skin. Redness, tenderness and generalized protrusion into the image commonly found. Incision and drainage immediately without waiting fluctuations, as in other subcutaneous infection, preventing the expansion of serius3.
It is important to know that there is no role of conservative medical therapy for rectal abscess. Anorektum abscess should be considered a surgical emergency and delay in surgical therapy resulted in further tissue damage. Multilateral expansion may extend into the thigh, scrotum, and even the abdominal wall, if surgical therapy ditunda3.
The principle is relatively simple surgical therapy. Under anesthesia with sigmoidoscopy or the evaluation of external and internal fingers, abscess drainage areas with simple excision and abscess cavity was left open. It is important to carefully explore the abscess cavity and surrounding tissue using a finger, because the finger-like protrusions may extend into the surrounding tissue, causing multiple abscesses, all of which must be opened and didrainase3.
Figure 1. Fistula ani 2
Sepsis can be started on intersfingter space and can be spread through 3 cara4:
1. Vertically
Figure 2. 4 Vertical Spread
2. In Horizontal
Figure 3. Horizontal Spread 4
3. In circumferential
Typically, three names are the consequences of the spread of abscesses in the direction of the above:
1. Perianal - sepsis spread vertically down the hall intersphincter,
adjacent to the anal canal as a perianal abscess
2. Ischiorectal - sepsis and appears to cross the sphincter externus away from the anal canal
as an ischiorectal abscess.
3. Supralevator - sepsis crossing vertically upwards causing collection
in supralevator.
Among these three routes, sepsis can also be present in the circumferential plane, causing horizontal4 collection.
IV. LAY fistula
Most fistula has a border estuary kripta anus and rectum and another hole in the skin of the perineum perianal1.
Fistula can be located in the subcutaneous, submucosal, antarsfingter, or through the sphincter. Fistula can be located anterior, lateral, or posterior. The form may be straight, curved, or similar to horseshoes. Sphincter are generally single, sometimes found the kompleks1.
Law Goodsall
To help examiners estimate the direction of the channel and the possible location of the internal estuary, can be used Goodsall Law. When the patient is in a position litotomi2:
If the external estuary located anterior of an imaginary line drawn from the anterior canal ani, fistula usually goes straight to anal kanal2.
If the external estuary is located next to the posterior of the line, fistula usually form the arch to the center line of the canal ani2.
Figure 4. Seton2 Figure 5. 1. kripta primary hole, 2. Hole sekunder3
Fistula with an aperture kripta generally shaped anterior straight. Fistula from the hole next to the dorsal kripta generally not straight, but bent forward due to inflammation and pus anterior pushed around m.puborektalis and may form one or more perforation holes anterior to, within the law Goodsall1. Various anatomical differences of abscess and fistula may occur, understanding it is facilitated by the spread of knowledge about routes infeksi4.
What are the key external fistula mouth of the estuary internal position
Common pathway fistulosa anorektum tract. Estuary internal (primary) is almost always in kripta; fistula usually involves only a single, muscular sphincter section; fistula compound or fistula involving the entire external sphincter muscular less prevalent. Goodsall law is transversal line dividing the anal fistula into two groups: (1). If the secondary estuary is located anterior to the transverse line that divides the anal canal into the anterior and posterior, usually associated with the mouth of the estuary is the primary through the tract fistulosa curved horseshoe or semi poultice kuda3.
It should be noted, however, the further away from the mouth of the external anal Goodsall the law can not be trusted. In addition, the direction of the fistula tract can not be diprediksi2 complex.
V. CLASSIFICATION fistula
Perianal fistula Park2 named by classification:
1. Fistula Transsphingter
Fistula is caused by an abscess transsphinkter ischiorektal, the expansion path through external sphingter. Happens about 25% of all fistula2.
The main lines crossing the sphincter externus contained on any level below the lowest fibers of the puborectalis to externus4 sphincter.
Figure 6. Fistula Transsphingter 5
Figure 7. Fistula transphingter2 Figure 8. Fistula Transsphingter4
2. Fistula Intersphingter
Intersphingter limited on space and internal sphingter. Caused by a perianal abscess. Happens about 70% of all fistula2. All of inflammatory pathways in the medial position striated sphincter muscle or externus4.
Figure 9. Fistula Intersfingter 5 Figure 10. Fistula Intersfingter 2
3. Fistula Suprasfingter
Abscess caused by supralevator. Passing the levator ani muscles, the height puborektal muscle and into the space intersphingter. Occurred about 5% of all fistula2. Very rarely, and the main lines crossing through levator ani4.
Figure 11. Fistula Suprasfingter 5
Figure 12. Fistula Suprasfingter 2 Figure 13. Fistula Suprasfingter 4
4. Fistula Ekstrasphingter
Not passing canal sphingter ani and mechanisms, through ischiorektal fossa and levator ani muscle, and empties rektum.Terjadi high about 1% of all fistula2. usually due to sepsis intrapelvis or improper operation of the surgical fistula others, and track complex beyond all sphincter4.
Figure 14. Fistula Ekstrasfingter5
Figure 15. Fistula Ekstrasfingter 2 Figure 16. Fistula Ekstrasfingter 4
VI. CLINICAL SYMPTOMS fistula
Fistula suspected apabila4:
- Persistent discharge at the site of drainage of abscesses
- Found intestinal organisms from culture results
- Recurrent abscesses occur
- Induration detected either clinically or in anesthesia
A history of repeated ani abscess drainage is an indication that someone may have fistula4. Usually the symptoms are limited to intermittent swelling, drainage, pruritus and discomfort varies. History is useful in diagnosis4 abscess.
A history of recurrent perianal abscess with an interval of time between them, along with spending a little pus.
Estuary externa is usually seen as red dots, inflamed, pus issued a mixed darah6, tinja2. Estuary skin typically somewhat elevated, gray papillae of pink granulation tissue. In time, the formation of scar along the channel is becoming palpable. Sonde can sometimes be inserted through the fistula into the linea pektineus. Usually not nyeri3.
In general, digital rectal fistula can be palpated between finger in the anus (not in the rectum) and the thumb on the perineal skin as thick as a rope about 3 mm (rectal bidigital). If the fistula rather straight to disonde up sonde out in kripta origin.
Perineal fistula rarely cause systemic disruption. Chronic fistula ages can undergo malignant degeneration into squamous skin planoseluler.
VII. EXAMINATION PENUNJANG6
Location estuary provide clues for possible external fistula track and sometimes fistula can be felt as a thickened line. In many cases, to see the track takes a lot of tools, and sometimes the path was not clear until surgery.
The equipment can be used by physicians:
1. Fistula probe. The tools are specifically made to put in fistula
2. Anoscope. Small instruments to see ani canal.
If the fistula complicated or located in an unusual place, may be used:
1. Diluted methylene blue dye. Injected into the fistula.
2. Fistulography. Entering the contrast fluid, and then photographed.
3. Magnetic resonance imaging
To rule out other disorders such as ulcerative colitis or Crohn's disease, may be used:
1. Flexible sigmoidoscopy.
The slim, flexible tube with a camera on the end, be able to view the rectum and sigmoid colon as the image layer yangdiperbesar on television.
2. Colonoscopy. Similar to sigmoidoscopy, but with the ability to examine the entire colon and small intestine.
VIII. MANAGEMENT
a. Perianal abscess
Antibiotics have little role because it can not penetrate into the pussy, and there is often fatty tissue necrosis. Acute abscesses requiring surgical drainage. It is not wise to do anything further though we suspect a fistula. - Swollen and hiperemis covering the exact location of the sphincter. Pus should always be sent for microbiological examination for the presence of intestinal organisms indicates a trend toward fistula4.
b. MANAGEMENT fistula
The purpose of the Rx is to heal the fistula with the least possible effect on the sphincter muscle. Planning will depend on the location of the fistula and its complexity, and the sphincter muscle strength pasien6. Management based on the eradication of sepsis with anal seoptimum may maintain function. Line fistula should be opened and allowed to recover from the bottom. The majority of superficial and intersphincter fistula (85%) directly diatasi4.
The rest (transphincteric and suprasphincteric) seem to be more difficult and require further specialist treatment. Usually the treatment is longer; carried out gradually to prevent damage sphincter4.
The operation aims menginsisi over fistula tract, leaving the incision open for granulating tesebut later. Usually achieved by placing the sonde through both the mouth of the fistula and a cut above the sonde. If the fistula followed the journey that requires cutting the sphincter, the incision should be cut perpendicular to the muscle fibers and only on one level. When incontinence arise if more than one muscle cut tempat3.
Fine monofilament thread (seton) often placed melalai primary paths around the sphincter externa as a temporary wound drain next to the exterior width of the sphincter externus striated muscle suffered penyembuhan4.
1. Fistulotomy
The surgeon first triangulate to find the mouth of the internal fistula. Then, the surgeon cuts and let the track in an open, mungkuretnya (removing it), then put a side to side so that the fistula was left open incision (flattened) flattenedout6.
To repair the fistula is more complicated, as Horshoe fistula (where the track passes around two sides of the body and has an external estuaries on both sides of the anus), the surgeon may leave open only on segments where the track together and issued sisanya6 path.
If a lot of that had to cut the sphincter muscle, surgery can be done in more than one phase and should be repeated if the entire line has not been able ditemukan6.
Techniques are left open (Fistulotomi) useful to the majority of fistula repair. In this procedure, a probe is inserted through the fistula (through both the mouth), and the skin covered them, subcutaneous tissue, and sphincter muscles are separated, so it opens up the channels. Curettage done to move the granulation tissue at the base of the channel. This technique is done carefully to avoid cutting too much sphincter (which can lead to incontinence). Fistulotomi left sekunder2 closes.
In fistula to do fistulotomi or fistulektomi. It is advisable to do as much as possible in fistulotomi, meaning fistula opened from original hole to shell hole. Heal wounds left open so that starting from the basic per sekundam intentionem. The wound will usually heal within a rather short time. Sometimes it takes a two-stage operation to avoid terpotongnya anus4 sphincter.
2. Rectal Flap
Sometimes, in order to reduce the amount of sphincter muscle that cut, the surgeon can remove the track and make a flap to the abdominal wall to reach and remove the internal fistula estuary. The flap is then affixed to the belakang6.
3. Seton Placement
The surgeon uses a seton untuk6:
- Creating a network around the muscle sphincter paurt before cutting
with a knife
- Allow seton to slowly cut through the muscle around the track
for several weeks.
Seton also help drainage fistula
Figure 17. Seton2
In patients with complex fistulas, recurrent fistula, Crohn's disease, imunokompromised state, seton can be used alone, or in combination with fistulotomi2.
Seton made from silk yarns are great, silastik marker, or a rubber band, which is mounted on the fistula tract and provide three objectives. The first one, we can look directly into the channel, the drain and triggers fibrin, and also cut through the fistula. therefore, over time, in line with the above seton fibrosis. Gently cut through the sphincter muscle, and reveal the channel. Seton diketatkan during a visit to the poly until he was pulled for more than 6-8 weeks. An advantage of using seton, is that "gradual fistulotomi" allows for the progressive division of the sphincter muscle, inkontinensia2 avoid complications.
4. Fibrin glue or collagen plugs
In some cases, doctors may use fibrin glue, made of a plasma protein, to clog and heal fistulas rather than cut and leave it open. The doctor injects glue through the external opening after clearing the channel in advance and put holes in the order closed. Fistula tract can also be blocked by the protein collagen and then ditutup6.
IX. Diagnosis APPEAL
Hidradenitis supurativa an inflammation of apocrine glands that usually form multiple subcutaneous fistula is sometimes found in the perineal and perianal. The disease is usually found in the armpits and generally does not extend to deeper structures dalam4.
Sinus pilonidalis sakrokoksigeal are just at the crease and from the nest hair from the dorsal end of the bone or bone koksigeus sakrum4.
Proctitis fistula can occur in Morbus Crohn, tuberculosis, amubiasis, fungal infections, and diverticulitis. Sometimes koloperineal fistula caused by a foreign object or trauma4.
Figure 18. Sinus Pilonidalis2
X. Prognosis
Fistula can recur if the hole did not participate in the open or removed, opened a branch fistula abstention, or skin wound was closed before reaching permukaan4 granulation tissue.
Failure of an optimal healing may akibat4:
- Inadequate initial therapy
- The specific cause (but not diagnosed), eg Crohn's Disease
- The condition is not good nutrition
- Which is not good wound care, for instance: a bridge epithelial
- Proliferation of granulation tissue which prevents epithelialization
If the three main causes have been eliminated, depending on the success of fistula surgery wound care operasi4 post.
REFERENCES
1. Sjamsuhidayat R, Wim de Jong, Buku Ajar Ilmu Bedah,
Edisi 2, Jakarta ,
EGC, 2005
hal : 677-678
2. http://www. fitsweb.uchc.edu/.../anorectal_fistula
3. Sabiston,
Buku Ajar Ilmu Bedah, bagian II, cetakan ke-dua, EGC, Jakarta , 1995, hal :
59-62
4. Henry MM,
Thompson JN , Principles of Surgery, 2nd edition, Elsevier
Saunders,
2005, page 423-426
5. http://img.medscape.com/pi/emed/ckb/general_surgery/188616-190234-3223.jpg
6. http://www.mayoclinic.org/anal-fistula/.html
7. Schwartz,
Shires, Spencer, Intisari Prinsip-prinsip Ilmu Bedah, Edisi 6, EGC, Jakarta,
hal : 426 – 427.











No comments:
Post a Comment