CHAPTER I
INTRODUCTION
Breast tumors often give the impression of scary, especially when found in women aged over 40 years. Even many of the oncologists argue that any tumor in the breast carcinoma, especially in women considered at high risk groups such as fibroadenoma, although benign tumors, dysplasia (fibrocystic, adenosis), mastitis and fat necrosis can not be ignored. This opinion is understandable, given the frequency of breast carcinomas are relatively high, giving rise to the problem health dala especially for women, not only in developed countries, but also in developing countries including Indonesia. The frequency of breast carcinoma in developed countries is the most that is the ratio of 5:1, compared with carcinoma of the cervix uteri, while in Indonesia ururtan neoplasms are located in the second after the cervix uteri karsinomaa.


CHAPTER II
Anatomy and Physiology
I. ANATOMY OF BREAST
The stroma of breast masses and breast parenchyma located in the anterior wall of the piston between the ICS II and VI and parasternal line to axilaris medius. Breasts consist of alveoli, lactiferous duct, lactiferous sinus, ampulla, pore pailla, and alveola edge. The main vascularization of the breast have a branch. the internal mammary, a. torakoakromialis and a branch. Intercostal.
Breast lies on either side hemitoraks with limits as follows:
A. Boundaries of the breast that looks from the outside:
a. Superior: ribs II or III
b. Inferior: VI or VII ribs
c. Medial: the edge of the sternum
d. Lateral: anterior axillary line
2. The boundaries of real breasts:
a. Superior: almost to the clavicle
b. Medial: midline
c. Lateral: m. latissimus dorsi
Figure 1. Anatomy of the breast
Figure 2.
Breast consists of various structures that parenkhim epithelial, fat, blood vessels, nerves and lymph salura and muscle and fascia. Parenkhim epithelial terentuk approximately 15-20 lobes, each of which has its own channel to drain the product, and comes down to your nipple. Each lobe is formed by lobule-lobule, each consisting of 10-100 asini group. Lobule-lobule is the basic structure of the mammary gland. Breast is covered by the pectoral fascia of the anterior and posterior surfaces which are connected cooper ligament that serves as a buffer. Cooper's ligament allowing greater mobility of the posterior side of the breast while providing structural support to the breast lobules and parenkima components.
With muskulokutis and fat components, mamma occupy the third and seventh ribs and extending to the width of the linea axillaris anterior parasternalis or media. Prevalent breast tissue will extend into the fold "axillary tail of Spence". Gland in the male component and duktulus mamma still rudimentary and poorly developed with short ducts and acini grown imperfect.
Mamma ektodermis remaining adults showed modification of the sweat glands to modification, so it is limited to the superficial and deep layers of the superficial fascia of the anterior chest wall. The deep layer of superficial fascia crosses the room to work retromammae pectoralis fascia (deep). Space known as the stock firmly on the side of the posterior retromamma breast, between the deep layer of superficial fascia and the fascia of musculus pectoralis major is embedded. The exchanges that promote the mobility of the breast to the chest wall. 2/3 breast are closely linked and attached to the fascia of the musculus pectoralis major. Condensation of dense fascia ligament clavipectoralis known as Halsted (costoclaviculare ligament) extends from the medial part of the first rib clavicula to just below this ligament runs through the subclavian artery and vein thoraxis apetura superior.
Non-lactating breast has a weight between 150-225 grams weight, whereas the lactating breast can be more than 500 grams.
I.1 vascularization BREAST
A. Arteries
Had bleeding from the breast:
a. A perforating branch. internal mammary. Branch I, II, III, IV penetrated the chest wall near the edge of the sternum in the intercostal appropriate, through the mayor and give m.pektoralis bleeding edge medial mammary gland.
b. Rami pectoralis a. thorako abdominalis. This artery runs down between the m. pectoralis minor and m. pectoralis major. This vessel is the main vessel m. pectoralis major. These vessels mendarahi part in the mammary gland.
c. A. thorako lateral (external mammary a.). These vessels run lateral edge mneyusuri m. mendarahi pectoralis major to the lateral breast.
d. A. thorako dorsalis. Is a branch of a. subscapularis. The artery mendarahi m. latissimus dorsi and m. serratus magna. Although this does not give the bleeding artery in the mammary gland, but it is very important. Because the action Radika; mastectomy, bleeding caused by arterial rupture is difficult to control, so the elapsed is called the bloody triangle.
Figure 3. Vascularization of breast
I.2 innervation
The nerves of the breast skin is maintained by the cervical plexus branch and n.interkostalis. Breast gland tissue itself is maintained by sympathetic nerves. There are some nerves again to keep in mind in connection with the complications of paralysis and numbness after surgery, ie, n. n.kutaneus interkostobrakialis and the care of the sensibility brakius medial axillary region. In the axillary nerve dissection is difficult to be removed so that frequent numbness in the area.
Nerve n. the care of the pectoral m. pectoralis major and minor, n. torakodorsalis who take care of m. latissimus dorsi and n. the care of the thoracic longus m. serratus anterior as far as possible be maintained at mastectomy with axillary dissection.
I.3 lymph vessels
Penyaliran lymph from the breast approximately 75% of the axillary glands of some to the parasternal, especially of the medial and setral and some are penyaliran to interpektoralis gland. In the axilla there are on average 50 (range 10-90 pieces) pieces of lymph nodes that are in addition to the brachial artery and vein. Channel to drain the lymph from the breast of the anterior axillary group, central group of axillary, the axillary part in passing along the axillary vein and continuing to the caudal cervical glands in the supraklavikuler.
Other lymphoid lines derived from central and medial areas are in addition to a. also the internal mammary to the contralateral axilla, to m. rectus muscle via ligamentum falciparum abdominilis hepatis to the liver, the pleura and to the contralateral breast.
Primary axillary lymph node group:
A. Externa mammary group. Arteria thoracica lateralis traveling parallel to the ribs from the sixth to the axillary vein and occupy the lateral edge of the musculus pectoralis major and medial axillary space.
2. Subscapularis group (scapularis). Close branches and blood vessels thracodorsalis subscapularis. He stretches of axillary vein to the lateral thorax wall.
3. Axillary vein group. Located most lateral, and many groups of lymph axilla. He is the central and caudal to the axillary vein.
4. Central lymph node groups. Centrally located between the anterior and posterior axilla LIPA and placed under the skin and superficial fascia medioaxilla.
5. Subclavicularis. Lymph node groups the highest and most medial. It is situated at the junction with the axillary vein subclavian vein as high as ligamnetum Halsted.
II. BREAST PHYSIOLOGY
Throughout his life, the female breast and physiological changes that vary patalogis. This is mainly related to variations in hormone levels that occur before, during and after reproduction. Hormones that affect breast development is estrogen, progesterone, LH, FSH (follicle stimulating hormone) and prolactin. Estrogen and progesterone produced by the ovaries, LH and FSH secreted by the basophil cells located in the anterior hypophysis gland prolactin secreted by the cells while asidofil hypophysis.
A few days after birth most infants, both men and women showed enlargement of breast glands begin to secrete less and less colostrum and disappeared after about a week later. Then again infantile mammary gland, is not active.
Breast experienced three changes in the affected hormones.
The first change is the start of the lifetime of the child through puberty, fertility period, up to klimakterium and menopause. Since puberty influence of progesterone produced ekstrogen and ovarian and pituitary hormones, has led to growing ducts and the onset of asinus.3
The second change is the change in accordance with the menstrual cycle. Around the eighth day of menstruation and breast become bigger in the next few days before the menstrual period maximal enlargement. Sometimes the pain arising bumps and uneven. For several days before menstruation breast pain became so tense and physical examination, especially palpation, not possible. At the time a mammogram examination is not useful because the contrast is too large glands. Once menstruation begins, all berkurang.3
The third change occurs during pregnancy and lactation. In pregnancy the breasts become huge because lobul duct epithelium and alveolar ducts proliferate, and grow a new duct. Secretion of prolactin from the anterior pituitary hormones trigger lactation. The milk produced by the cells of the alveoli, filling the acini, and then expelled through the ducts to the nipple.
III. BREAST EMBRYOLOGY
In human embryos, the first breast is known as "milk steak" that grew around the sixth week of fetal development. An area of thickening ektodermis known as milk shoots, develops in the embryo pectoral body. This strictly linear elevation extending from bilateral axillae to the vulva and is known as the milk line or "mammary ridge".
After reaching the ninth week in the womb, milk line to atrophy, except in the pectoral region and breast primodrium first introduction into the nipple buds. Upon reaching the twelfth week, shoot the nipples ektodermis invaded by squamous epithelium. In the fifth, mesenchymal connective tissue infiltrating breast primordium and berdifrensiasi into dense filaments 15 to 20, are distributed symmetrically under the skin of the nipple bud.
Duktulus mammary develop as growth in the ventral than the rest of the embryology of this, which is divided into primary milk ducts and lobules end in the bud. These buds then proliferates into acini after start of ovarian estrogen stimulation. During growth in the uterus, the primary milk duct branching and splitting wide. By reaching the seventh and eighth months in utero, the ductus lumen berkanulasi form associated with lactiferous ducts did not mature.
At birth, shoot the nipples have a central basin corresponding to the area penetrated by the primary lumen duktulus milk. Immediately after birth, complete penetration of the nipple shoots, he bereversi and more invaded by basaloid cells which become dark dipigmentasi to form the areola.
CHAPTER III
Ca mammary
Ca mammary
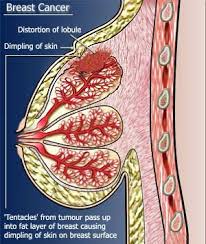
Ca mammary or breast cancer is a malignant tumor that grows in the breast tissue. Breast cancer is a group of abnormal cells in the breast that continues to grow and change menjadiganas. Eventually these cells to form lumps in the breast. Cancer can begin to grow in the milk glands, milk ducts, fatty tissue and connective tissue in the breast.
If the cancerous lump is not removed or controlled, cancer cells can spread (metastasis) to other body parts. Metastases may occur in lymph nodes (lymph) in the armpit or the shoulder blade. In addition to cancer cells lodged in bone, lung, liver, skin, and under the skin.
EPIDEMIOLOGY
Incidence of breast cancer in the last decade show an increasing trend. This is expected due to the better education and technology that have a broad impact in the discovery of the disease, the higher the state of socio-economic status also have an impact on changes in lifestyle.
In the U.S. (1983) 92 cases of breast cancer incidence of females with mortality baru/100.000 27/100.000 ie less than 18% of deaths in women. In Indonesia there is no breast cancer data, but a data base registration pathological noted that breast cancer was second (15.8%) of the ten largest cancer after cervical cancer.
Distribution according to tumor location berdasrkan research (Hagensen) breast cancer is more common in the upper lateral quadrant, then the central (subareolar). The left breast is more frequently affected than the right.
Distribution by age, breast cancer is more common at age 40-49 years (decades V) which is 30.35% for cases in Indonesia; in Japan so that 40.6% of breast cancers are found at the age of 40-49 years ( V decade).
World Health Organization (WHO) states that the top five cancers in the world is lung cancer, breast cancer, colon cancer and gastric cancer and liver cancer. While data from pathological examination in Indonesia stated that the order of the top five cancer is cervical cancer, breast cancer, lymph nodes, skin and nasopharyngeal cancer, breast cancer is the cancer most affects women is about 32% of all malignancies in women.
The death rate from breast cancer in females reach 5 million. Breast cancer is the highest cause of cancer death in women is approximately 19% .5 Recent data suggest that breast cancer deaths in women showed the second highest cause of death after cancer of the uterus. Usually found in women aged 40-49 years. Located on the upper lateral quadrant.
TYPE OF BREAST CANCER
1.Karsinoma in situ
Carcinoma in situ means that cancer is still in place, an early cancer that has not spread or infiltrate out of the place of origin.
2.Karsinoma ductal
Ductal carcinomas originate from cells that line the channel leading to the nipple. Approximately 90% of breast cancer is ductal carcinoma. These cancers usually occur before or after the menopause. Sometimes this cancer can be touched, and on the mammogram, the cancer appears as small spots of calcium deposits (microcalcifications).
This cancer is usually limited to certain areas in the breast as a whole and can be removed surgically. Approximately 25-35% of patients with ductal carcinoma will develop invasive cancer (usually in the same breast).
3.Karsinoma lobuler
Carcinoma lobuler begin growing in the mammary gland, usually occurs after menopause. This cancer can not be felt and not seen on mammogram, but it is usually found incidentally on mammography performed for other purposes. Approximately 25-30% of patients with carcinoma lobuler will eventually invasive cancer.
4.Kanker invasive
Invasive cancer is cancer that has spread and damage other tissues, can be localized (confined to the breast) or metastatic (spread the body gets more). Approximately 80% of breast cancers are invasive ductal cancer and 10% were lobular cancer.
5.Karsinoma medullary
Cancer is derived from the mammary gland
6.Karsinoma tubular
Cancer is derived from the mammary gland.
RISK FACTORS
Increased exposure to estrogen is associated with increased risk of developing breast cancer, which can be considered to reduce exposure to protect. Accordingly, factors that increase the number of menstrual cycles, such as early menarche, nuliparitas, and late menopause, is associated with increased risk. A moderate exercise levels and an extended lactation period, the factors that menurungkan the menstrual cycle is protecting. Terminal differentiation of breast epithelium is associated with full-time pregnancy is also protected, so that older age at first birth diakitkan with increased incidence of breast cancer. Finally, there is a correlation between obesity and increased breast cancer. Because the main source of estrogen in postmenopausal women is a result of conversion of androstenedione to estrone by adipose tissue, obesity is associated with long-term estrogen exposure meningktnya.
Included is a nonhormonal risk of radiation exposure. Young women who got radiation therapy had Hodgkin's lymphoma of breast cancer risk 75 times more than the subjects in the study based on matching age. The study also mengukapkan number and duration Cleaner in consuming alcohol diakitkan with increased risk of breast cancer. Alcohol consumption is known to increase serum levels of estradiol.
The cause is unknown, but there are some risk factors that cause a woman to be more likely to suffer from breast cancer
Some risk factors are:
1.Usia
As in many types of cancer, the incidence by age rises with age.
2.Keluarga
Of epidemiology seem that likely to suffer breast cancer two to three times greater in women whose mother or sibling with breast cancer. This possibility is greater when the mother or siblings have cancer or premenopausal bilateral.
Women who had dealt with breast carcinoma, it has got a high risk of breast carcinoma in another.
3.Hormonal
Breast cancer growth is often affected by changes in hormone balance. High levels of hormones during the reproductive period of women, especially if not interrupted by hormonal changes in pregnancy, seems to increase the chances of growth of cells that are genetically damaged and cause cancer.
4.Menarke (first menstruation) before age 11, menopause after age 55 years, first pregnancy after age 30 years or had never been pregnant.
The earlier the menarche, the greater the risk of breast cancer. Similarly, the first pregnancy or menopause. The slower the menopause and first pregnancy, the greater the risk of breast cancer.
5.Pemakaian birth control pills or estrogen replacement therapy
Birth control pills may slightly increase breast cancer risk, which depends on age, length of usage and other factors. Is not known how long the effects will still be there after pill use is stopped the pill.
Estrogen replacement therapy lived for over 5 years seems also slightly increase the risk of breast cancer and the risk is increased if its use is much longer.
6.Obesitas post-menopausal
Some studies suggest obesity as a risk factor for breast cancer, possibly because of high levels of estrogen in obese women
7.Pemakaian alcohol
The use of alcohol more than 1-2 cups / day can increase the risk of breast cancer.
Chemical 8.Bahan
Several studies have cited the exposure of chemicals that mimic estrogen (found in pesticides and other industrial products) may increase the risk of breast cancer.
9.Penyinaran
Exposure to radiation (especially radiation to the chest), in childhood may increase the risk of breast cancer.
10.Faktor other risk
Several studies have shown that cervical cancer, ovarian and colon cancer and a history of cancer in the family can increase the risk of breast cancer.
It is noteworthy that a high risk factor is not the etiologic factor. By knowing the risk factors in a person's expected that he was more aware of the abnormalities that exist in the breast, either by carrying out routine and periodic breast self examination of breast abnormalities or no abnormalities to the doctor. And for doctors to perform a good physical examination and mammography examination legeartis and in patients with high risk factors.
The aim is simply to be more vigilant, not to scare and cause anxiety in people who have these factors. In addition there are iu some of these risk factors are primarily for those who have abnormalities mammari dysplasia, not married and so on. In case this is not advisable to take medications and birth control pills in women with dysplasia or mammari in women over 35 years.
Based on these risk factors and see also the factors that contributed to the etiology of breast cancer is not impossible that this could also dihidari (or prevented), although in a limited sense.
Indications Mammography:
- Evaluation of doubtful lumps or changes in breast vague.
- If ever there is a contralateral breast carcinoma of the breast
- Looking for a primary carcinoma when there is metastasis, while the source is unknown.
- Screening of mammary carcinoma at high risk.
- Screening of prior acts of plastic or cosmetic surgery.
Etiology BREAST CANCER
Etiology of breast cancer we do not know for sure because it is multifactorial.
There are several suspected risk factors associated with breast cancer, namely:
Height. Height exceeding 170 cm. 170 cm tall woman who has breast cancer risk due to faster growth at the age of children and adolescents to make a change in genetic structure (DNA) in body cells that include changes to the malignant cells.
Age. Age above 30 years old or over 35 years. Approximately 60% of breast cancers occur in over 60 years. The greatest risk found in women aged over 75 years.
pregnancy history. The first pregnancy after age 30.
History of childbirth. First child at the age above 35 years.
History of marriage. Not / never married.
nulliparous. Nulliparous (women who have had children). Longer exposed to the hormone estrogen is relatively much longer than women who already have children.
History of menarche. Age of menarche (first menstruation) under 12 years old or under 10 years.
menopausal age above 55 years old or over 60 years.
History of infection or trauma.
history of breast cancer and a history of benign breast tumor surgery. After the affected breast removed, then the risk of breast cancer in a healthy increase of 0.5 -1% / year.
Never suffer from non-cancerous breast disease.
hormonal factors and hormonal therapy for long.
contralateral breast cancer.
History of gynecologic surgery, such as ovarian tumor.
History of radiation in the chest area.
genetic factors. Family history of breast cancer, for example, mother, sibling (sister or mother's sister. Has 2-3 times greater risk for breast cancer.
oral contraceptives in patients with benign fibrocystic breasts as a malignant disorder.
Use of birth control pills or estrogen replacement therapy. Use of preparations for, or more than 5 years.
overweight and obese women after menopause. With weight loss, body estrogen levels will drop too.
The use of alcohol. The use of alcohol more than 1-2 cups / day can increase the risk of breast cancer.
Chemicals. Several studies have cited the exposure of chemicals that mimic estrogen (which is contained in pesticides and other industrial products) may increase the risk of breast cancer.
DES (diethylstilbestrol). Women who took DES to prevent miscarriages have a high risk of breast cancer.
BREAST CANCER PATHOPHYSIOLOGY
Breast cancer is not the only disease but many, depending on the affected breast tissue, estrogen dependence, and age of beginning. Malignant breast disease before menopause is different from malignant breast disease after menopause (postmenopausal). Treatment response and prognosis in contrast to many other dangerous diseases.
Some tumors are known as "estrogen dependent" contain receptors that bind estradiol, a type of estrogen, and growth is stimulated by estrogen. These receptors are not the manual on normal breast tissue or in tissue with dysplasia. The presence of tumor "Estrogen Receptor Assay (ERA)" on the network is higher than breast cancers are hormone dependent. These cancers respond to hormone treatment (endocrine chemotherapy, oophorectomy, or adrenalectomy).
CLASSIFICATION OF BREAST CANCER
In breast cancer staging is based on the UICC TNM classification system in 2002
Stage 0 Tis N0 M0
T1 N0 M0 Stage I
T0 N1 M0 Stage IIA
T1 N1 M0
T2 N0 M0
T2 N1 M0 stage IIB
T3 N0 M0
Stage IIIA N2 M0 T0
T1 N2 M0
T2 N2 M0
T3 N1 M0
T3 N2 M0
T4 N0 M0 Stage IIIB
T4 N1 M0
T4 N2 M0
Stage IIIC Any T N3 M0
Stage IV Any T Any N M1
It is also established diagnostic examination required at each stage are:
Cancer Staging
0 I II III IV
History and PF x x x x x
CBC, platelet x x x x
Liver function x x x x
Photo chest x x x x
Bilateral mammogram x x x x x
Hormone receptor status x x x x
A bone scan x x x
Ultrasound, CT or MRI abdomen x x
Primary tumor (T):
A. Tx: Primary tumor can not be determined
2. T0: No evidence of primary tumor
3. Tis: The cancer in situ, Paget dis with no palpable tumor at the papilla
4. T1: Tumor <2 cm
a. T1A: Tumor <0.5 cm
b. T1b: Tumor 0.5 to 1 cm
c. T1c: Tumor 1-2 cm
5. T2: Tumor 2-5 cm
6. T3: Tumor more than 5 cm
7. T4: Tumor regardless of the size, spread directly into the wall of the thorax or the skin:
a. T4a: Attached to the chest wall
b. T4b: Edema of the skin, ulceration, peau d'orange, satellite
c. T4c: T4a and T4b
d. T4d: Mastitis carcinomatosis
Regional lymph nodes (N):
A. Nx: regional glandular enlargement can not be determined
2. N0: Not palpable glands axila
3. N1: axila homolateral palpable enlargement of the gland that is not attached
4. N2: axila homolateral palpable enlarged lymph attached to each other or attached to surrounding tissue
5. N3: There is homolateral internal mammary lymph
Metastas distant (M):
A. Mx: distant metastasis can not be determined
2. M0: No distant metastasis
3. M1: There is a distant metastasis, including lymph subklavikula
STADIUM BREAST CANCER
Breast cancer has four stages, namely:
Stage I: Tumor less than 2 cm in diameter without lymph node involvement (LN) and without distant spread. Tumor confined to the breast and not fixed to the skin and pectoral muscles.
Stage IIa: The tumor is less than 2 cm in diameter with lymph node involvement (LN) and without distant spread or tumor with a diameter of approximately 5 cm with no lymph node involvement (LN) and without distant spread.
Stage IIb: The tumor with a diameter of approximately 5 cm with involvement of lymph nodes (LN) and without distant spread or tumor over 5 cm in diameter without lymph node involvement (LN) and without distant spread.
Stage IIIa: Tumor more than 5 cm in diameter with lymph node involvement (LN) without distant spread.
Stage IIIb: The tumor diameter over 5 cm with involvement of lymph nodes (LN) and there is distant spread of metastases to the supraclavicular lymph node involvement (LN) metastasis to supraclavicular or infraclavicular or infiltrate / spread to the skin or chest wall or tumor with edema on the hands .
Stage IV: Tumor that have distant metastases
Figure 4. Stadium Ca
Performance status (performance status) cancer according to WHO (1979):
0: Good, can work normally.
1: Simply, can not work hard but work can be mild.
2: Weak, unable to work but able to walk and care for themselves 50% of the time conscious.
3: Bad, can not walk, can get up and take care of yourself, need to lie down over 50% of the time conscious.
4: Awful, can not get up and unable to care for yourself, just lie down.
Performance status (performance status) according to Karnofsky cancer:
100%: Able to carry out normal activities, complaints / disorders do not exist.
90%: No need special care, minimally symptomatic complaints.
80%: No special treatment by some of the complaints / symptoms.
70%: Not able to work but able to care for themselves.
60%: Do not need help but can generally be done for its own purposes.
50%: Need help and generally need drugs.
40%: Not able to care for themselves, need special care and assistance.
30%: Need consideration of hospice care.
20%: severe pain, need hospital treatment.
10%: Approaching death.
0%: Died. "Rest in peace & no pain".
The largest tumor size was found to be 2 cm (95.24%). Stage breast cancer is found most stage IIIb (35.71%). The majority of positive axillary lymph nodes (47.63%). Histopathological picture of ductal (90.48%) and poor differentiation degree (40.48%) .5 Karnofsky less 60%, not worth it given sitostatika.
Hematogenous metastasis of breast cancer:
The location of the main symptoms and signs
Brain Headache, nausea, vomiting, epilepsy, ataxia, paresis, paresthesias
Pleural effusion, shortness of breath
Usually no symptoms of pulmonary
Sometimes no symptoms of heart
Mass, obstructive jaundice
Bones:
- Skull
- Vertebra
- Ribs
- The long bone
CLINICAL BREAST CANCER
Early symptoms include a lump that is usually perceived differently than the surrounding breast tissue, painless and usually have an irregular edge. In the early stages, when driven by a finger, a lump can be moved easily under the skin. In later stages, the lump is usually attached to the chest wall or the surrounding skin. In advanced cancer, may develop a swollen lump or breast skin ulcers. Sometimes the skin over the lump shrank and looked like an orange peel.
Patients usually present with a lump / mass in the breast, there may also be pain without pain, an abnormal discharge from the nipple (usually bloody or yellow to green, perhaps purulent), skin disorders arise in the form of changes in skin color or texture (dimpling, redness, ulceration, peau d'orange) of the breast, nipple and areola (dark brown colored area around the nipple) and the wound did not heal for a long time.
Figure 5. Dimpling
Figure 6. Peau de orange
Other symptoms that may be found in a lump or mass in the armpit, change the size or shape of the breast, the skin around the nipple scaly or no indentation of the skin, nipples are interested in (retraction of the nipple) or itching or swelling of one breast. Consistency is hard and dense breasts, lump demarcated with a size less than 5 cm, usually in this stage there has been no spread of cancer cells beyond the breast.
Enlarged lymph nodes or distant metastasis mark. In later stages may develop bone pain, weight loss, swelling of arms or skin ulceration. Any abnormality in the breast should be considered malignant until we prove it is not malignant.
PHYSICAL EXAMINATION
a. Anamnesis
A lump in the breast is a major complaint of patients. At first no pain, but further growth will occur in complaining of pain. Rapid growth of malignant tumors is possible. Cough or shortness of breath may occur in cases where tumor metastasis to the lung. Malignant tumors of the breast accompanied by pain in the waist to think about the possibility of bone metastasis in the vertebrae. In the case of the dubious history more focused on risk group indications
Pain is a physiological that arise before or after menstruation, and is felt in both breasts. Benign tumors such as retention cysts or other benign tumor, is almost painless. Even in the stage of breast cancer permulaanpun painless. We feel the pain that had started to infiltrate into the surrounding
b. Physical examination
Breast physical examination should be done with a gentle manner and should not be rough and hard. Not infrequently the cause petechlenecehymoses under harsh kulit.orang ill with malignant lesions should not be repeatedly examined by a doctor or student because of the possibility of the spread
Should be done first by hand on the side and after that with his hands up, with the patient sitting.
Figure 7. Realize
On inspection it can be seen through the dilated blood vessels under the skin due to enlargement of benign or malignant tumor under the skin
Can be seen:
- There are more hard lump attached or fixed to.
- The nipples drawn into.
- Eczema on the nipple.
- Edema.
- Peau d'orange.
- Ulceration, satellite tumors in the skin.
- Discharge from the nipple
- Asymmetrical breasts.
- Enlarged axillary lymph nodes.
Figure 8. Ca mammary
Palpation
Palpation must include the entire breast, from parasternal towards the axillary line to the rear, from the most distal direction subklavikular (Wiknjosastro Hanifa, 1994).
Palpation performed by using the palm of the fingers 3-4. Palpation of the peripheral soft start to the areola and nipple.
SUPPORT BREAST CANCER DIAGNOSIS
Investigations for diagnosis of breast cancer include:
A. Mammography and / or breast ultrasound.
2. X-ray.
3. Fine needle aspiration (FNAB) of breast tumors.
4. Ultrasound liver / abdomen.
5. A complete blood chemistry examination in preparation for surgery.
6. Bone scan or bone survey.
7. Chemical examination of blood / tumor marker: CEA, Ca 15-3, CA 125.
Ultrasound is usually used to distinguish tumor with a cyst difficult. Mammography is the examination that can see the internal structure of the breast, this is early detection of tumors or cancer.
To determine the occurrence of metastasis, we can do a chest X-ray, bonesurvey, ultrasound abdominal / liver ultrasound and CT. Scan. CT. Scan is used for the diagnosis of breast carcinoma metastasis to other organs. Other tests were hematologic examination. Hematological examination is by way of isolation and determining the tumor cells in blood circulation and sentrifugis sedimental blood. Joint investigation between the ultrasound and mammography provide a higher diagnostic accuracy.
BREAST CANCER DIAGNOSIS
In the anamnesis, we ask about risk factors for breast cancer patients and the influence of the menstrual cycle to complaints or changes in tumor size. To minimize the influence of estrogen and progesterone, the examination should do ± 1 week calculated starting from the first day of menstruation.
Examination techniques that we do as follows, namely:
A. Sitting position
Perform inspection checks the position of the patient's hand to the side and free fall
± the same examiner stood in front of the patient's height. Consider the state of the left and right breast, symmetrical / not; there any abnormalities of papillae, the location and shape, nipple retraction, skin disorders of peau d'orange, dimpling, ulceration or signs of inflammation.
Do well in the position of the patient's arm shot up to see if there is a shadow
tumor under the skin that come to move or is there a part that remains, dimpling and others.
2. A lying position
We recommend that the patient back pillows propped up. Perform palpation examination that we started from the cranial region as high as the second rib to rib height distal to-6. Perform well in the same way subaerolar and papillae. Doing all the centrifuges. Finally, apply pressure on the papilla area to see if there is discharge.
Set the state of a tumor based on the quadrant tumor location, tumor size, consistency
tumor, tumor extent whether or not the firm, and the mobility of tumors to the skin, pectoral muscle or chest wall.
Perform examination of regional lymph nodes in the axilla, supraclavicular,
infraclavicular, and neck. Do also check other organs to determine the presence or absence of metastasis. Organs include the liver, spleen, spine, and lung paru1.
Symptoms of distant metastasis among others:
The brain: headache, nausea, vomiting, epilepsy, ataxia, paresis, and paralysis.
Lung: effusion, and shortness of breath.
Liver: sometimes asymptomatic, jaundice mass obstruction.
Bones: pain and fractures.
Breast cancer diagnosis is made by:
A. Confirm the diagnosis of malignancy: clinical examination, FNA and imaging (mammography and / or breast ultrasound). (Tripple diagnostic).
2. Stage diagnosis of breast cancer: clinical examination, laboratory tests and
imaging (ultrasound images toraks/paru- liver/abdomen- k / p bone scanning). In the situation where one component of a triple diagnostic experience discrepancies biopsy interpretation is done by examination of frozen pieces (if there are facilities) or biopsy are used to determine the type histopatologinya. Breast cancer diagnosis can only be enforced by histopathological examination. Subsequent therapy depends on the outcome histopatologinya.
Histopathologic examination can be done in two ways, namely:
A. Excision biopsy. Excision biopsy is done by lifting all the tumor tissue and less in surrounding healthy tissue. This action is performed on the tumor with a diameter of approximately 5 cm.
2. Incisional biopsy. Incisional biopsy is done by lifting some of the tumor tissue and less in surrounding healthy tissue. This action is performed on an inoperable tumor or
diameter over 5 cm.
BREAST CANCER PREVENTION
Many risk factors can not be controlled. Some dietitians and oncologists believe that changes in diet and lifestyle in general can reduce the incidence of cancer. Endeavored to make early diagnosis of breast cancer easier to treat and can disembuhan if it is still at an early stage. Be aware, clinical breast examination and mammography as a screening procedure is 3 tools to detect cancer early. Need to know, that 9 out of 10 women found a lump in her breast. For primary prevention, it can be done alone. Examination should be done after the menstrual period is completed. Before menstruation, breast slightly swollen making it difficult for the examination. The way the examination is as follows:
A. Stand in front of the mirror and see if there are abnormalities in the breast. Usually these two are not the same breast, the nipple is not located at the same height. Notice if there are wrinkles, grooves, or the nipples are interested. When there is disorder or blood or discharge from the nipple, immediately go to the doctor.
2. Put your arms above your head and look back to the breast.
3. Bend to the breast hanging down, and check again.
4. Lie in bed and put your left hand behind his head, and a pillow under your left shoulder. Touch the left breast with the palm of the right radius. Check if there are lumps in the breast. Then check whether there is a lump or swelling in the left armpit.
5. Check and Touch the nipple and surrounding areas. In general, the mammary glands when touched with your fingers will feel rubbery and easily moved. If there is a tumor, it will feel hard and can not be moved (not to be moved from its place). If you feel there is a lump the size of 1 cm or more, immediately go to the doctor. The earlier treatment, more likely to recover completely. Do the same for breast and right armpit.
TREATMENT OF BREAST CANCER
Before planning a mamma carcinoma therapy, clinical and pathological diagnosis as well as the diffusion rate should be ascertained first. Clinical diagnosis should be similar to the histopathologic diagnosis. If they are different, must be determined which one was wrong. If the purpose curative, it is a consequence of radical action must be done to cure mutilation. But when the follow-surgical palliative actions are useless.
Usually treatment is started after a thorough assessment of the condition of the patient, which is about 1 week or more after the biopsy. Rx consists of surgical and non surgical. Non-surgical therapy consisted of radiation therapy, chemotherapy, hormonal therapy and endocrine. Form of hormone therapy and hormone inhibitors.
Surgery
To get a histological diagnosis of biopsy is usually done so that action can be regarded as the first act in mamma surgery. With frozen preparations, the results can be obtained within 15 minutes. If the examination shows signs of a benign tumor, then the operation is completed, but the results showed a malignant tumor, the operation can proceed with curative surgery.
Surgery is possible curative radical mastectomy, modified radical surgery and conservative surgical excision of the tumor is large.
Always conservative surgery plus axillary lymph node dissection and radiotherapy in the (remaining) breast. Three such measures are a package of treatment that should be implemented simultaneously. In short it is called a therapeutic treatment to preserve the breast.
Curative therapy is performed if the tumor is confined to the breast and there was no infiltration into the chest wall, skin of mamma, or infiltration of the lymph nodes to surrounding structures. If the tumor is called capable agkat with radical surgical follow the entire tumor and its spread in the lymph nodes can be removed. Surgery is done according to the Halstead radical which includes the removal of the breast with most of the skin, m.pektoralis major and minor glands of the armpit and all at once. This is the standard surgical Pemebedahan since the beginning of the 20th century until the '50s.
After the sixties radical surgery is usually performed as modified by Patey. In this operation m. pectoralis major and the minor is maintained if the tumor is free of the obvious mommy muscles.
Curative surgery is now usually done by maintaining the breast. Absolute requirement for this operation is a small tumor and the availability of specific radiotherapy (megavolt) for irradiation. Irradiation is needed to prevent recurrence of the tumor in the breast tumor tissue is left behind or from another tumor nests (multicentric carcinoma).
Thus at the last moment dilakuka usually modified radical surgery (Patey). If it is possible and available means of postoperative irradiation, it is recommended that treatment is a lumpectomy breast maintains extensive axillary lymph node dissection with.
Palliative Surgery in breast cancer is almost never done. Sometimes a solitary residif lokoregional excised, but usually at first have seemed a solitary, but sebenarnnya has spread, so that removal of the tumor is often not useful residif. Amputation is sometimes performed on mamma gland tumor that was not able to lift because of its size and has been estimated by radiotherapy. Although the goal of palliative therapy is sometimes nothing works for quite mean.
Radiotherapy
Radiotherapy in breast cancer is usually used in the curative therapy by maintaining a mamma and as adjunctive therapy or palliative therapy.
Curative radiotherapy as monotherapy lokoregional ineffective, but as an adjunct therapy for curative intent in a relatively large tumor may be useful.
Palliative radiotherapy can be performed with good results for a limited time when the tumor was not able to raise locally. Called tumor could not lift when it reaches the level of T4.
Breast Cancer Radiation Therapy
Radiation therapy is used to kill cancer cells in the removal of the tumor
and the surrounding area, including the lymph nodes (lymph nodes) that can not be resected regional in advanced cancer; in bone metastases, axillary lymph node metastases.
Breast Cancer Chemotherapy
Chemotherapy (a combination of drugs to kill cells that proliferate with
fast or pressing breeding) and drug-hormone inhibitors (drugs that
affect the hormones that promote cancer cell growth) are used to suppress the growth of cancer cells throughout the body. As adjuvant systemic chemotherapy after palliative mastectomy in advanced disease.
Breast Cancer Surgery
Breast cancer surgery called mastectomy. Types of mastectomy:
A. Partial mastectomy (local tumor excision and irradiation). Ranging from lumpectomy to
segmental removal (removal of an extensive network with the affected skin).
2. Total mastectomy with low axial dissection of the entire breast, lymph node dilateral otocpectoralis all minor.
3. Radical mastectomy. The entire breast, pectoralis major and minor muscles underneath: the entire axial.
4. A modified radical mastectomy (Modified Radical Mastectomy).
5. Extended radical mastectomy. Just as radical mastectomy plus internal mammary lymph nodes.
Modified Radical Mastectomy is a surgical oncologist at the malignancy
the breast is to remove the entire breast tissue, all or most of the axial network consisting of stroma and parenkhim entire breast, areola and nipple and the skin over the tumor with axillary lymph node dissection ipsilateral level I, II / III is en bloc without lifting m . pectoralis major and minor.
Indications of operation:
A. Early-stage breast cancer (stage I and II).
2. Locally advanced breast cancer with certain requirements.
3. Soft tissue malignancy of the breast.
Contraindication of operation:
A. Tumor attached to the chest wall.
2. Edema of the arm.
3. Extensive satellite nodules.
4. Inflamatoar mastitis.
Operative action depends on the stage of breast cancer, namely:
A. Breast Cancer Stage I and II
Management of breast cancer stage I and II with radical mastectomy or
modification. Continue with the provision of regional radiation and adjuvant chemotherapy in breast cancer has undergone metastasis. Allegations of metastasis can be determined by examination of the lymph nodes. Simplex mastectomy can we give anyway. Mastectomy should be accompanied by radiation to the tumor bed and regional lymph node regions.
Surgery in T2N1 breast cancer is accompanied by a radical mastectomy radiation
in the local tumor bed and regional lymph nodes. Management of any tumor located in the central or medial quadrant of the breast should be accompanied by radiation in the chain of regional lymph nodes.
Other alternatives can be performed on small tumors Breast conserving therapy techniques. This technique is in the form of a package consisting of removal of the tumor only (tumorektomi) that axillary dissection and radiation with curative (approximately 3 cm tumor size) with certain conditions. How this is done with a wedge excision, segmental resection, partial resection, kwadranektomi, or regular lumpectomy, followed by axillary lymph node dissection in total.
The terms of technique Breast conserving therapy:
A. Primary tumor is not more than 2 cm.
2. N1b is less than 2 cm.
3. There are currently no distant metastasis.
4. No other primary tumor.
5. Contralateral breast cancer free.
6. Breast concerned have never received prior treatment (except lumpectomy).
7. Not performed on small breasts because the cosmetic result is not very prominent.
8. Primary tumor is localized behind the nipple.
2. Stage IIIA Breast Cancer
Management of stage IIIa breast cancer with radical mastectomy, followed
with adjuvant chemotherapy. Simplex or mastectomy followed by radiotherapy to the tumor bed provision and regional lymph nodes.
Modified Radical Mastectomy Technique (Modified Radical Mastectomy)
In brief, the operation technique of modified radical mastectomy (Modified Radical
Mastectomy) can be explained as follows:
A. Patients in general anesthesia, ipsilateral to the operated arm is positioned
900 abduction, shoulder ipsilateral to the operated fouled thin pillow.
2. Disinfection of the operating field, the top until the middle of the neck, the bottom
up to the umbilicus, the contralateral medial to the mid mammma, the
lateral to the lateral edge of the scapula. Disinfected circular upper arm up to
elbow is then wrapped with sterile doek followed by narrowing the field
operation with doek sterile.
3. If found ulcers in breast tumors, the ulcer should be covered with sterile gauze thick (Buick Gaas) and circular stitches.
4. Made an incision (incisional variety is Stewart, Orr, Willy Meyer, Halsted, incisions S) where the line of incision at least within 2 cm from the edge of the tumor, then the flap is created.
5. Flap top to below the clavicle, medially to the parasternal ipsilateral flap, flap down
to the inframammary fold, lateral flap to the anterior edge of m. Latissimus dorsi and identify and vasa. N. Thoracalis dorsalis.
6. Mastectomy starts from the medial to lateral while caring for bleeding, especially branches of blood vessels in the parasternal intercostal. At the time until the lateral edge of m. Haak pectoralis major with the help of mamma tissue removed from the m. Pectoralis minor and serratus anterior (simple mastectomy). In the radical mastectomy pectoral muscle has begun.
7. Axillary dissection begins with finding an enlarged axillary lymph nodes Level I (lateral m.
pectoralis minor), Level II (behind the m. pectoralis minor) and level III (medial m. pectoralis minor). Dissection is not higher in vasa axillary region, because it can lead to edema of the arm. Veins leading to the network mamma ligated. Further identify vasa and n. Thoracalis longus, and thoracalis dorsalis, interkostobrachialis. The next internerural didiseksi KGB and eventually the network regardless mamma and axillary lymph nodes as a single unit (en bloc).
8. The operating field and washed with a solution of Nacl 0.9% sublimat.
9. All the tools are used during surgery was replaced with a new set, as well as
handschoen operator, assistant and instruments as well as doek sterility.
10.Evaluasi re-sources of bleeding.
11.Dipasang 2 pieces drain, large drain (Redon no. 14) is placed below the vasa axillary,
drain is smaller (12) is directed to the medial.
12.Luka lapais closed operation by layer.
Complications of Surgery
Early complications:
A. Bleeding.
2. Lesion n. Thoracalis longus à wing scapula.
3. Lesion n. Thoracalis dorsalis.
Complications Slow
A. Infections.
2. Flap necrosis.
3. Wound dehiscence.
4. Seroma.
5. Edema of the arm.
6. Stiffness of the shoulder joint contractures à.
Palliative actions Breast Cancer
Management is still operabel / kurabel up on stage IIIa. Management
breast cancer stage IIIb and IV is no longer a mastectomy instead of palliative treatment.
Palliative actions aimed at further stages:
A. Maintaining the quality of life of patients in order to keep good / high and regard death
is a normal process.
2. Not accelerate or postpone death.
3. Relieve pain or other complaints are disturbing.
Palliative care is based on the stages, namely:
A. Breast Cancer Stage IIIb
Palliative treatment of breast cancer stage IIIb incisional biopsy and radiation followed.
If the residue does not exist, wait. If relapse, add to the hormonal treatment and chemotherapy. However, when residue remained after radiation, hormonal treatment is given immediately as follows:
In premenopausal patients, bilateral oophorectomy do.
In patients who have 1-5 years of menopause, check the effects of estrogen. If the effect is positive, do it like no. A. If the effect is negative, do it like no. 3. Observation for 6-8 weeks. If a positive response, continue treatment but if the response is negative, do chemotherapy with CMF (CAF) at least 12 cycles for 6 weeks.
In postmenopausal patients, hormonal therapy did inhibitif / additives.
2. Breast Cancer Stage IV
Palliative treatment of stage IV breast cancer, namely:
A. In the premenopausal patients, bilateral oophorectomy do. When a positive response, give or tamofen aminoglutetimid. If relapse or negative response, given CMF chemotherapy (CAF).
2. In patients who have 1-5 years of menopause, check the effects of estrogen. Effects of estrogen can be checked with the estrogen / progesterone receptors (ER / PR). If the effect is positive, do it like no. A. If the effect is negative, do it like no. 31.
3. In the postmenopausal patient, do hormonal therapy, like tamoxifen, estrogen, progesterone, or corticosteroids.
Description: C = cyclophosphamide, M = methotrexate, F = 5-fluourasil.
FOLLOW UP BREAST CANCER
Year 1 and 2 controls every 2 months.
Year 3 s / d 5 control every 3 months.
After 5 years of control every 6 months.
Physical examination: every time control.
Thorax photo: every 6 months.
Lab. Marker: every 2-3 months.
contralateral Mammography: every year or there is any indication.
USG abdomen every 6 months or there is any indication.
Bone scanning: every 2 years or no indication.
APPEAL BREAST CANCER DIAGNOSIS
Differential diagnosis of breast cancer, among others:
A. Mammary fibroadenomas (FAM). Mammary fibroadenoma is a benign breast tumor
commonly found in younger age (15-30 years) with a dense chewy consistency, well defined, painless and cars. Adequate therapy with excision.
2. Fibrocystic disorders. The disorder is benign fibrocystic payudara6 with
solid rubbery consistency / cystic, not demarcated, there is pain, especially before menstruation,
increase in size, usually bilateral / multiple. Medical therapy with symptomatic.
3. Phylodes tumors both malignant and benign, like kistosarkoma filoides. Kistosarkoma filoides resemble mammary fibroadenoma (FAM) are large, oval, well defined, and the car. Can reach 20-30 cm in size. Treatment is with simple mastectomy.
4. Galactocele. Galactocele a cystic tumor mass due to blockage of the channel / lactiferous ducts. These tumors are found on the new mother / nursing.
5. Extensive mastitis. Mastitis is an infection of the breast with a complete inflammatory signs.
Mastitis can develop into an abscess. Mastitis is usually found in women who are breastfeeding. Mastitis is broad, especially in tuberculous mastitis.
6. Other malignancies of the breast (sarcoma, lymphoma, etc.).
CHAPTER IV
CONCLUSION
By looking at the journey of breast neoplasia as the stage through which it can be concluded that early detection of breast cancer can develop methods of breast self examination, clinical breast examination, mammography, ultrasound and computerized tomography. While breast cancer diagnosis can be established by clinical examination, cytology and biopsy.
REFERENCES
INTRODUCTION
Breast tumors often give the impression of scary, especially when found in women aged over 40 years. Even many of the oncologists argue that any tumor in the breast carcinoma, especially in women considered at high risk groups such as fibroadenoma, although benign tumors, dysplasia (fibrocystic, adenosis), mastitis and fat necrosis can not be ignored. This opinion is understandable, given the frequency of breast carcinomas are relatively high, giving rise to the problem health dala especially for women, not only in developed countries, but also in developing countries including Indonesia. The frequency of breast carcinoma in developed countries is the most that is the ratio of 5:1, compared with carcinoma of the cervix uteri, while in Indonesia ururtan neoplasms are located in the second after the cervix uteri karsinomaa.
CHAPTER II
Anatomy and Physiology
I. ANATOMY OF BREAST
The stroma of breast masses and breast parenchyma located in the anterior wall of the piston between the ICS II and VI and parasternal line to axilaris medius. Breasts consist of alveoli, lactiferous duct, lactiferous sinus, ampulla, pore pailla, and alveola edge. The main vascularization of the breast have a branch. the internal mammary, a. torakoakromialis and a branch. Intercostal.
Breast lies on either side hemitoraks with limits as follows:
A. Boundaries of the breast that looks from the outside:
a. Superior: ribs II or III
b. Inferior: VI or VII ribs
c. Medial: the edge of the sternum
d. Lateral: anterior axillary line
2. The boundaries of real breasts:
a. Superior: almost to the clavicle
b. Medial: midline
c. Lateral: m. latissimus dorsi
Figure 1. Anatomy of the breast
Figure 2.
Breast consists of various structures that parenkhim epithelial, fat, blood vessels, nerves and lymph salura and muscle and fascia. Parenkhim epithelial terentuk approximately 15-20 lobes, each of which has its own channel to drain the product, and comes down to your nipple. Each lobe is formed by lobule-lobule, each consisting of 10-100 asini group. Lobule-lobule is the basic structure of the mammary gland. Breast is covered by the pectoral fascia of the anterior and posterior surfaces which are connected cooper ligament that serves as a buffer. Cooper's ligament allowing greater mobility of the posterior side of the breast while providing structural support to the breast lobules and parenkima components.
With muskulokutis and fat components, mamma occupy the third and seventh ribs and extending to the width of the linea axillaris anterior parasternalis or media. Prevalent breast tissue will extend into the fold "axillary tail of Spence". Gland in the male component and duktulus mamma still rudimentary and poorly developed with short ducts and acini grown imperfect.
Mamma ektodermis remaining adults showed modification of the sweat glands to modification, so it is limited to the superficial and deep layers of the superficial fascia of the anterior chest wall. The deep layer of superficial fascia crosses the room to work retromammae pectoralis fascia (deep). Space known as the stock firmly on the side of the posterior retromamma breast, between the deep layer of superficial fascia and the fascia of musculus pectoralis major is embedded. The exchanges that promote the mobility of the breast to the chest wall. 2/3 breast are closely linked and attached to the fascia of the musculus pectoralis major. Condensation of dense fascia ligament clavipectoralis known as Halsted (costoclaviculare ligament) extends from the medial part of the first rib clavicula to just below this ligament runs through the subclavian artery and vein thoraxis apetura superior.
Non-lactating breast has a weight between 150-225 grams weight, whereas the lactating breast can be more than 500 grams.
I.1 vascularization BREAST
A. Arteries
Had bleeding from the breast:
a. A perforating branch. internal mammary. Branch I, II, III, IV penetrated the chest wall near the edge of the sternum in the intercostal appropriate, through the mayor and give m.pektoralis bleeding edge medial mammary gland.
b. Rami pectoralis a. thorako abdominalis. This artery runs down between the m. pectoralis minor and m. pectoralis major. This vessel is the main vessel m. pectoralis major. These vessels mendarahi part in the mammary gland.
c. A. thorako lateral (external mammary a.). These vessels run lateral edge mneyusuri m. mendarahi pectoralis major to the lateral breast.
d. A. thorako dorsalis. Is a branch of a. subscapularis. The artery mendarahi m. latissimus dorsi and m. serratus magna. Although this does not give the bleeding artery in the mammary gland, but it is very important. Because the action Radika; mastectomy, bleeding caused by arterial rupture is difficult to control, so the elapsed is called the bloody triangle.
Figure 3. Vascularization of breast
I.2 innervation
The nerves of the breast skin is maintained by the cervical plexus branch and n.interkostalis. Breast gland tissue itself is maintained by sympathetic nerves. There are some nerves again to keep in mind in connection with the complications of paralysis and numbness after surgery, ie, n. n.kutaneus interkostobrakialis and the care of the sensibility brakius medial axillary region. In the axillary nerve dissection is difficult to be removed so that frequent numbness in the area.
Nerve n. the care of the pectoral m. pectoralis major and minor, n. torakodorsalis who take care of m. latissimus dorsi and n. the care of the thoracic longus m. serratus anterior as far as possible be maintained at mastectomy with axillary dissection.
I.3 lymph vessels
Penyaliran lymph from the breast approximately 75% of the axillary glands of some to the parasternal, especially of the medial and setral and some are penyaliran to interpektoralis gland. In the axilla there are on average 50 (range 10-90 pieces) pieces of lymph nodes that are in addition to the brachial artery and vein. Channel to drain the lymph from the breast of the anterior axillary group, central group of axillary, the axillary part in passing along the axillary vein and continuing to the caudal cervical glands in the supraklavikuler.
Other lymphoid lines derived from central and medial areas are in addition to a. also the internal mammary to the contralateral axilla, to m. rectus muscle via ligamentum falciparum abdominilis hepatis to the liver, the pleura and to the contralateral breast.
Primary axillary lymph node group:
A. Externa mammary group. Arteria thoracica lateralis traveling parallel to the ribs from the sixth to the axillary vein and occupy the lateral edge of the musculus pectoralis major and medial axillary space.
2. Subscapularis group (scapularis). Close branches and blood vessels thracodorsalis subscapularis. He stretches of axillary vein to the lateral thorax wall.
3. Axillary vein group. Located most lateral, and many groups of lymph axilla. He is the central and caudal to the axillary vein.
4. Central lymph node groups. Centrally located between the anterior and posterior axilla LIPA and placed under the skin and superficial fascia medioaxilla.
5. Subclavicularis. Lymph node groups the highest and most medial. It is situated at the junction with the axillary vein subclavian vein as high as ligamnetum Halsted.
II. BREAST PHYSIOLOGY
Throughout his life, the female breast and physiological changes that vary patalogis. This is mainly related to variations in hormone levels that occur before, during and after reproduction. Hormones that affect breast development is estrogen, progesterone, LH, FSH (follicle stimulating hormone) and prolactin. Estrogen and progesterone produced by the ovaries, LH and FSH secreted by the basophil cells located in the anterior hypophysis gland prolactin secreted by the cells while asidofil hypophysis.
A few days after birth most infants, both men and women showed enlargement of breast glands begin to secrete less and less colostrum and disappeared after about a week later. Then again infantile mammary gland, is not active.
Breast experienced three changes in the affected hormones.
The first change is the start of the lifetime of the child through puberty, fertility period, up to klimakterium and menopause. Since puberty influence of progesterone produced ekstrogen and ovarian and pituitary hormones, has led to growing ducts and the onset of asinus.3
The second change is the change in accordance with the menstrual cycle. Around the eighth day of menstruation and breast become bigger in the next few days before the menstrual period maximal enlargement. Sometimes the pain arising bumps and uneven. For several days before menstruation breast pain became so tense and physical examination, especially palpation, not possible. At the time a mammogram examination is not useful because the contrast is too large glands. Once menstruation begins, all berkurang.3
The third change occurs during pregnancy and lactation. In pregnancy the breasts become huge because lobul duct epithelium and alveolar ducts proliferate, and grow a new duct. Secretion of prolactin from the anterior pituitary hormones trigger lactation. The milk produced by the cells of the alveoli, filling the acini, and then expelled through the ducts to the nipple.
III. BREAST EMBRYOLOGY
In human embryos, the first breast is known as "milk steak" that grew around the sixth week of fetal development. An area of thickening ektodermis known as milk shoots, develops in the embryo pectoral body. This strictly linear elevation extending from bilateral axillae to the vulva and is known as the milk line or "mammary ridge".
After reaching the ninth week in the womb, milk line to atrophy, except in the pectoral region and breast primodrium first introduction into the nipple buds. Upon reaching the twelfth week, shoot the nipples ektodermis invaded by squamous epithelium. In the fifth, mesenchymal connective tissue infiltrating breast primordium and berdifrensiasi into dense filaments 15 to 20, are distributed symmetrically under the skin of the nipple bud.
Duktulus mammary develop as growth in the ventral than the rest of the embryology of this, which is divided into primary milk ducts and lobules end in the bud. These buds then proliferates into acini after start of ovarian estrogen stimulation. During growth in the uterus, the primary milk duct branching and splitting wide. By reaching the seventh and eighth months in utero, the ductus lumen berkanulasi form associated with lactiferous ducts did not mature.
At birth, shoot the nipples have a central basin corresponding to the area penetrated by the primary lumen duktulus milk. Immediately after birth, complete penetration of the nipple shoots, he bereversi and more invaded by basaloid cells which become dark dipigmentasi to form the areola.
CHAPTER III
Ca mammary
Ca mammary
Ca mammary or breast cancer is a malignant tumor that grows in the breast tissue. Breast cancer is a group of abnormal cells in the breast that continues to grow and change menjadiganas. Eventually these cells to form lumps in the breast. Cancer can begin to grow in the milk glands, milk ducts, fatty tissue and connective tissue in the breast.
If the cancerous lump is not removed or controlled, cancer cells can spread (metastasis) to other body parts. Metastases may occur in lymph nodes (lymph) in the armpit or the shoulder blade. In addition to cancer cells lodged in bone, lung, liver, skin, and under the skin.
EPIDEMIOLOGY
Incidence of breast cancer in the last decade show an increasing trend. This is expected due to the better education and technology that have a broad impact in the discovery of the disease, the higher the state of socio-economic status also have an impact on changes in lifestyle.
In the U.S. (1983) 92 cases of breast cancer incidence of females with mortality baru/100.000 27/100.000 ie less than 18% of deaths in women. In Indonesia there is no breast cancer data, but a data base registration pathological noted that breast cancer was second (15.8%) of the ten largest cancer after cervical cancer.
Distribution according to tumor location berdasrkan research (Hagensen) breast cancer is more common in the upper lateral quadrant, then the central (subareolar). The left breast is more frequently affected than the right.
Distribution by age, breast cancer is more common at age 40-49 years (decades V) which is 30.35% for cases in Indonesia; in Japan so that 40.6% of breast cancers are found at the age of 40-49 years ( V decade).
World Health Organization (WHO) states that the top five cancers in the world is lung cancer, breast cancer, colon cancer and gastric cancer and liver cancer. While data from pathological examination in Indonesia stated that the order of the top five cancer is cervical cancer, breast cancer, lymph nodes, skin and nasopharyngeal cancer, breast cancer is the cancer most affects women is about 32% of all malignancies in women.
The death rate from breast cancer in females reach 5 million. Breast cancer is the highest cause of cancer death in women is approximately 19% .5 Recent data suggest that breast cancer deaths in women showed the second highest cause of death after cancer of the uterus. Usually found in women aged 40-49 years. Located on the upper lateral quadrant.
TYPE OF BREAST CANCER
1.Karsinoma in situ
Carcinoma in situ means that cancer is still in place, an early cancer that has not spread or infiltrate out of the place of origin.
2.Karsinoma ductal
Ductal carcinomas originate from cells that line the channel leading to the nipple. Approximately 90% of breast cancer is ductal carcinoma. These cancers usually occur before or after the menopause. Sometimes this cancer can be touched, and on the mammogram, the cancer appears as small spots of calcium deposits (microcalcifications).
This cancer is usually limited to certain areas in the breast as a whole and can be removed surgically. Approximately 25-35% of patients with ductal carcinoma will develop invasive cancer (usually in the same breast).
3.Karsinoma lobuler
Carcinoma lobuler begin growing in the mammary gland, usually occurs after menopause. This cancer can not be felt and not seen on mammogram, but it is usually found incidentally on mammography performed for other purposes. Approximately 25-30% of patients with carcinoma lobuler will eventually invasive cancer.
4.Kanker invasive
Invasive cancer is cancer that has spread and damage other tissues, can be localized (confined to the breast) or metastatic (spread the body gets more). Approximately 80% of breast cancers are invasive ductal cancer and 10% were lobular cancer.
5.Karsinoma medullary
Cancer is derived from the mammary gland
6.Karsinoma tubular
Cancer is derived from the mammary gland.
RISK FACTORS
Increased exposure to estrogen is associated with increased risk of developing breast cancer, which can be considered to reduce exposure to protect. Accordingly, factors that increase the number of menstrual cycles, such as early menarche, nuliparitas, and late menopause, is associated with increased risk. A moderate exercise levels and an extended lactation period, the factors that menurungkan the menstrual cycle is protecting. Terminal differentiation of breast epithelium is associated with full-time pregnancy is also protected, so that older age at first birth diakitkan with increased incidence of breast cancer. Finally, there is a correlation between obesity and increased breast cancer. Because the main source of estrogen in postmenopausal women is a result of conversion of androstenedione to estrone by adipose tissue, obesity is associated with long-term estrogen exposure meningktnya.
Included is a nonhormonal risk of radiation exposure. Young women who got radiation therapy had Hodgkin's lymphoma of breast cancer risk 75 times more than the subjects in the study based on matching age. The study also mengukapkan number and duration Cleaner in consuming alcohol diakitkan with increased risk of breast cancer. Alcohol consumption is known to increase serum levels of estradiol.
The cause is unknown, but there are some risk factors that cause a woman to be more likely to suffer from breast cancer
Some risk factors are:
1.Usia
As in many types of cancer, the incidence by age rises with age.
2.Keluarga
Of epidemiology seem that likely to suffer breast cancer two to three times greater in women whose mother or sibling with breast cancer. This possibility is greater when the mother or siblings have cancer or premenopausal bilateral.
Women who had dealt with breast carcinoma, it has got a high risk of breast carcinoma in another.
3.Hormonal
Breast cancer growth is often affected by changes in hormone balance. High levels of hormones during the reproductive period of women, especially if not interrupted by hormonal changes in pregnancy, seems to increase the chances of growth of cells that are genetically damaged and cause cancer.
4.Menarke (first menstruation) before age 11, menopause after age 55 years, first pregnancy after age 30 years or had never been pregnant.
The earlier the menarche, the greater the risk of breast cancer. Similarly, the first pregnancy or menopause. The slower the menopause and first pregnancy, the greater the risk of breast cancer.
5.Pemakaian birth control pills or estrogen replacement therapy
Birth control pills may slightly increase breast cancer risk, which depends on age, length of usage and other factors. Is not known how long the effects will still be there after pill use is stopped the pill.
Estrogen replacement therapy lived for over 5 years seems also slightly increase the risk of breast cancer and the risk is increased if its use is much longer.
6.Obesitas post-menopausal
Some studies suggest obesity as a risk factor for breast cancer, possibly because of high levels of estrogen in obese women
7.Pemakaian alcohol
The use of alcohol more than 1-2 cups / day can increase the risk of breast cancer.
Chemical 8.Bahan
Several studies have cited the exposure of chemicals that mimic estrogen (found in pesticides and other industrial products) may increase the risk of breast cancer.
9.Penyinaran
Exposure to radiation (especially radiation to the chest), in childhood may increase the risk of breast cancer.
10.Faktor other risk
Several studies have shown that cervical cancer, ovarian and colon cancer and a history of cancer in the family can increase the risk of breast cancer.
It is noteworthy that a high risk factor is not the etiologic factor. By knowing the risk factors in a person's expected that he was more aware of the abnormalities that exist in the breast, either by carrying out routine and periodic breast self examination of breast abnormalities or no abnormalities to the doctor. And for doctors to perform a good physical examination and mammography examination legeartis and in patients with high risk factors.
The aim is simply to be more vigilant, not to scare and cause anxiety in people who have these factors. In addition there are iu some of these risk factors are primarily for those who have abnormalities mammari dysplasia, not married and so on. In case this is not advisable to take medications and birth control pills in women with dysplasia or mammari in women over 35 years.
Based on these risk factors and see also the factors that contributed to the etiology of breast cancer is not impossible that this could also dihidari (or prevented), although in a limited sense.
Indications Mammography:
- Evaluation of doubtful lumps or changes in breast vague.
- If ever there is a contralateral breast carcinoma of the breast
- Looking for a primary carcinoma when there is metastasis, while the source is unknown.
- Screening of mammary carcinoma at high risk.
- Screening of prior acts of plastic or cosmetic surgery.
Etiology BREAST CANCER
Etiology of breast cancer we do not know for sure because it is multifactorial.
There are several suspected risk factors associated with breast cancer, namely:
Height. Height exceeding 170 cm. 170 cm tall woman who has breast cancer risk due to faster growth at the age of children and adolescents to make a change in genetic structure (DNA) in body cells that include changes to the malignant cells.
Age. Age above 30 years old or over 35 years. Approximately 60% of breast cancers occur in over 60 years. The greatest risk found in women aged over 75 years.
pregnancy history. The first pregnancy after age 30.
History of childbirth. First child at the age above 35 years.
History of marriage. Not / never married.
nulliparous. Nulliparous (women who have had children). Longer exposed to the hormone estrogen is relatively much longer than women who already have children.
History of menarche. Age of menarche (first menstruation) under 12 years old or under 10 years.
menopausal age above 55 years old or over 60 years.
History of infection or trauma.
history of breast cancer and a history of benign breast tumor surgery. After the affected breast removed, then the risk of breast cancer in a healthy increase of 0.5 -1% / year.
Never suffer from non-cancerous breast disease.
hormonal factors and hormonal therapy for long.
contralateral breast cancer.
History of gynecologic surgery, such as ovarian tumor.
History of radiation in the chest area.
genetic factors. Family history of breast cancer, for example, mother, sibling (sister or mother's sister. Has 2-3 times greater risk for breast cancer.
oral contraceptives in patients with benign fibrocystic breasts as a malignant disorder.
Use of birth control pills or estrogen replacement therapy. Use of preparations for, or more than 5 years.
overweight and obese women after menopause. With weight loss, body estrogen levels will drop too.
The use of alcohol. The use of alcohol more than 1-2 cups / day can increase the risk of breast cancer.
Chemicals. Several studies have cited the exposure of chemicals that mimic estrogen (which is contained in pesticides and other industrial products) may increase the risk of breast cancer.
DES (diethylstilbestrol). Women who took DES to prevent miscarriages have a high risk of breast cancer.
BREAST CANCER PATHOPHYSIOLOGY
Breast cancer is not the only disease but many, depending on the affected breast tissue, estrogen dependence, and age of beginning. Malignant breast disease before menopause is different from malignant breast disease after menopause (postmenopausal). Treatment response and prognosis in contrast to many other dangerous diseases.
Some tumors are known as "estrogen dependent" contain receptors that bind estradiol, a type of estrogen, and growth is stimulated by estrogen. These receptors are not the manual on normal breast tissue or in tissue with dysplasia. The presence of tumor "Estrogen Receptor Assay (ERA)" on the network is higher than breast cancers are hormone dependent. These cancers respond to hormone treatment (endocrine chemotherapy, oophorectomy, or adrenalectomy).
CLASSIFICATION OF BREAST CANCER
In breast cancer staging is based on the UICC TNM classification system in 2002
Stage 0 Tis N0 M0
T1 N0 M0 Stage I
T0 N1 M0 Stage IIA
T1 N1 M0
T2 N0 M0
T2 N1 M0 stage IIB
T3 N0 M0
Stage IIIA N2 M0 T0
T1 N2 M0
T2 N2 M0
T3 N1 M0
T3 N2 M0
T4 N0 M0 Stage IIIB
T4 N1 M0
T4 N2 M0
Stage IIIC Any T N3 M0
Stage IV Any T Any N M1
It is also established diagnostic examination required at each stage are:
Cancer Staging
0 I II III IV
History and PF x x x x x
CBC, platelet x x x x
Liver function x x x x
Photo chest x x x x
Bilateral mammogram x x x x x
Hormone receptor status x x x x
A bone scan x x x
Ultrasound, CT or MRI abdomen x x
Primary tumor (T):
A. Tx: Primary tumor can not be determined
2. T0: No evidence of primary tumor
3. Tis: The cancer in situ, Paget dis with no palpable tumor at the papilla
4. T1: Tumor <2 cm
a. T1A: Tumor <0.5 cm
b. T1b: Tumor 0.5 to 1 cm
c. T1c: Tumor 1-2 cm
5. T2: Tumor 2-5 cm
6. T3: Tumor more than 5 cm
7. T4: Tumor regardless of the size, spread directly into the wall of the thorax or the skin:
a. T4a: Attached to the chest wall
b. T4b: Edema of the skin, ulceration, peau d'orange, satellite
c. T4c: T4a and T4b
d. T4d: Mastitis carcinomatosis
Regional lymph nodes (N):
A. Nx: regional glandular enlargement can not be determined
2. N0: Not palpable glands axila
3. N1: axila homolateral palpable enlargement of the gland that is not attached
4. N2: axila homolateral palpable enlarged lymph attached to each other or attached to surrounding tissue
5. N3: There is homolateral internal mammary lymph
Metastas distant (M):
A. Mx: distant metastasis can not be determined
2. M0: No distant metastasis
3. M1: There is a distant metastasis, including lymph subklavikula
STADIUM BREAST CANCER
Breast cancer has four stages, namely:
Stage I: Tumor less than 2 cm in diameter without lymph node involvement (LN) and without distant spread. Tumor confined to the breast and not fixed to the skin and pectoral muscles.
Stage IIa: The tumor is less than 2 cm in diameter with lymph node involvement (LN) and without distant spread or tumor with a diameter of approximately 5 cm with no lymph node involvement (LN) and without distant spread.
Stage IIb: The tumor with a diameter of approximately 5 cm with involvement of lymph nodes (LN) and without distant spread or tumor over 5 cm in diameter without lymph node involvement (LN) and without distant spread.
Stage IIIa: Tumor more than 5 cm in diameter with lymph node involvement (LN) without distant spread.
Stage IIIb: The tumor diameter over 5 cm with involvement of lymph nodes (LN) and there is distant spread of metastases to the supraclavicular lymph node involvement (LN) metastasis to supraclavicular or infraclavicular or infiltrate / spread to the skin or chest wall or tumor with edema on the hands .
Stage IV: Tumor that have distant metastases
Figure 4. Stadium Ca
Performance status (performance status) cancer according to WHO (1979):
0: Good, can work normally.
1: Simply, can not work hard but work can be mild.
2: Weak, unable to work but able to walk and care for themselves 50% of the time conscious.
3: Bad, can not walk, can get up and take care of yourself, need to lie down over 50% of the time conscious.
4: Awful, can not get up and unable to care for yourself, just lie down.
Performance status (performance status) according to Karnofsky cancer:
100%: Able to carry out normal activities, complaints / disorders do not exist.
90%: No need special care, minimally symptomatic complaints.
80%: No special treatment by some of the complaints / symptoms.
70%: Not able to work but able to care for themselves.
60%: Do not need help but can generally be done for its own purposes.
50%: Need help and generally need drugs.
40%: Not able to care for themselves, need special care and assistance.
30%: Need consideration of hospice care.
20%: severe pain, need hospital treatment.
10%: Approaching death.
0%: Died. "Rest in peace & no pain".
The largest tumor size was found to be 2 cm (95.24%). Stage breast cancer is found most stage IIIb (35.71%). The majority of positive axillary lymph nodes (47.63%). Histopathological picture of ductal (90.48%) and poor differentiation degree (40.48%) .5 Karnofsky less 60%, not worth it given sitostatika.
Hematogenous metastasis of breast cancer:
The location of the main symptoms and signs
Brain Headache, nausea, vomiting, epilepsy, ataxia, paresis, paresthesias
Pleural effusion, shortness of breath
Usually no symptoms of pulmonary
Sometimes no symptoms of heart
Mass, obstructive jaundice
Bones:
- Skull
- Vertebra
- Ribs
- The long bone
CLINICAL BREAST CANCER
Early symptoms include a lump that is usually perceived differently than the surrounding breast tissue, painless and usually have an irregular edge. In the early stages, when driven by a finger, a lump can be moved easily under the skin. In later stages, the lump is usually attached to the chest wall or the surrounding skin. In advanced cancer, may develop a swollen lump or breast skin ulcers. Sometimes the skin over the lump shrank and looked like an orange peel.
Patients usually present with a lump / mass in the breast, there may also be pain without pain, an abnormal discharge from the nipple (usually bloody or yellow to green, perhaps purulent), skin disorders arise in the form of changes in skin color or texture (dimpling, redness, ulceration, peau d'orange) of the breast, nipple and areola (dark brown colored area around the nipple) and the wound did not heal for a long time.
Figure 5. Dimpling
Figure 6. Peau de orange
Other symptoms that may be found in a lump or mass in the armpit, change the size or shape of the breast, the skin around the nipple scaly or no indentation of the skin, nipples are interested in (retraction of the nipple) or itching or swelling of one breast. Consistency is hard and dense breasts, lump demarcated with a size less than 5 cm, usually in this stage there has been no spread of cancer cells beyond the breast.
Enlarged lymph nodes or distant metastasis mark. In later stages may develop bone pain, weight loss, swelling of arms or skin ulceration. Any abnormality in the breast should be considered malignant until we prove it is not malignant.
PHYSICAL EXAMINATION
a. Anamnesis
A lump in the breast is a major complaint of patients. At first no pain, but further growth will occur in complaining of pain. Rapid growth of malignant tumors is possible. Cough or shortness of breath may occur in cases where tumor metastasis to the lung. Malignant tumors of the breast accompanied by pain in the waist to think about the possibility of bone metastasis in the vertebrae. In the case of the dubious history more focused on risk group indications
Pain is a physiological that arise before or after menstruation, and is felt in both breasts. Benign tumors such as retention cysts or other benign tumor, is almost painless. Even in the stage of breast cancer permulaanpun painless. We feel the pain that had started to infiltrate into the surrounding
b. Physical examination
Breast physical examination should be done with a gentle manner and should not be rough and hard. Not infrequently the cause petechlenecehymoses under harsh kulit.orang ill with malignant lesions should not be repeatedly examined by a doctor or student because of the possibility of the spread
Should be done first by hand on the side and after that with his hands up, with the patient sitting.
Figure 7. Realize
On inspection it can be seen through the dilated blood vessels under the skin due to enlargement of benign or malignant tumor under the skin
Can be seen:
- There are more hard lump attached or fixed to.
- The nipples drawn into.
- Eczema on the nipple.
- Edema.
- Peau d'orange.
- Ulceration, satellite tumors in the skin.
- Discharge from the nipple
- Asymmetrical breasts.
- Enlarged axillary lymph nodes.
Figure 8. Ca mammary
Palpation
Palpation must include the entire breast, from parasternal towards the axillary line to the rear, from the most distal direction subklavikular (Wiknjosastro Hanifa, 1994).
Palpation performed by using the palm of the fingers 3-4. Palpation of the peripheral soft start to the areola and nipple.
SUPPORT BREAST CANCER DIAGNOSIS
Investigations for diagnosis of breast cancer include:
A. Mammography and / or breast ultrasound.
2. X-ray.
3. Fine needle aspiration (FNAB) of breast tumors.
4. Ultrasound liver / abdomen.
5. A complete blood chemistry examination in preparation for surgery.
6. Bone scan or bone survey.
7. Chemical examination of blood / tumor marker: CEA, Ca 15-3, CA 125.
Ultrasound is usually used to distinguish tumor with a cyst difficult. Mammography is the examination that can see the internal structure of the breast, this is early detection of tumors or cancer.
To determine the occurrence of metastasis, we can do a chest X-ray, bonesurvey, ultrasound abdominal / liver ultrasound and CT. Scan. CT. Scan is used for the diagnosis of breast carcinoma metastasis to other organs. Other tests were hematologic examination. Hematological examination is by way of isolation and determining the tumor cells in blood circulation and sentrifugis sedimental blood. Joint investigation between the ultrasound and mammography provide a higher diagnostic accuracy.
BREAST CANCER DIAGNOSIS
In the anamnesis, we ask about risk factors for breast cancer patients and the influence of the menstrual cycle to complaints or changes in tumor size. To minimize the influence of estrogen and progesterone, the examination should do ± 1 week calculated starting from the first day of menstruation.
Examination techniques that we do as follows, namely:
A. Sitting position
Perform inspection checks the position of the patient's hand to the side and free fall
± the same examiner stood in front of the patient's height. Consider the state of the left and right breast, symmetrical / not; there any abnormalities of papillae, the location and shape, nipple retraction, skin disorders of peau d'orange, dimpling, ulceration or signs of inflammation.
Do well in the position of the patient's arm shot up to see if there is a shadow
tumor under the skin that come to move or is there a part that remains, dimpling and others.
2. A lying position
We recommend that the patient back pillows propped up. Perform palpation examination that we started from the cranial region as high as the second rib to rib height distal to-6. Perform well in the same way subaerolar and papillae. Doing all the centrifuges. Finally, apply pressure on the papilla area to see if there is discharge.
Set the state of a tumor based on the quadrant tumor location, tumor size, consistency
tumor, tumor extent whether or not the firm, and the mobility of tumors to the skin, pectoral muscle or chest wall.
Perform examination of regional lymph nodes in the axilla, supraclavicular,
infraclavicular, and neck. Do also check other organs to determine the presence or absence of metastasis. Organs include the liver, spleen, spine, and lung paru1.
Symptoms of distant metastasis among others:
The brain: headache, nausea, vomiting, epilepsy, ataxia, paresis, and paralysis.
Lung: effusion, and shortness of breath.
Liver: sometimes asymptomatic, jaundice mass obstruction.
Bones: pain and fractures.
Breast cancer diagnosis is made by:
A. Confirm the diagnosis of malignancy: clinical examination, FNA and imaging (mammography and / or breast ultrasound). (Tripple diagnostic).
2. Stage diagnosis of breast cancer: clinical examination, laboratory tests and
imaging (ultrasound images toraks/paru- liver/abdomen- k / p bone scanning). In the situation where one component of a triple diagnostic experience discrepancies biopsy interpretation is done by examination of frozen pieces (if there are facilities) or biopsy are used to determine the type histopatologinya. Breast cancer diagnosis can only be enforced by histopathological examination. Subsequent therapy depends on the outcome histopatologinya.
Histopathologic examination can be done in two ways, namely:
A. Excision biopsy. Excision biopsy is done by lifting all the tumor tissue and less in surrounding healthy tissue. This action is performed on the tumor with a diameter of approximately 5 cm.
2. Incisional biopsy. Incisional biopsy is done by lifting some of the tumor tissue and less in surrounding healthy tissue. This action is performed on an inoperable tumor or
diameter over 5 cm.
BREAST CANCER PREVENTION
Many risk factors can not be controlled. Some dietitians and oncologists believe that changes in diet and lifestyle in general can reduce the incidence of cancer. Endeavored to make early diagnosis of breast cancer easier to treat and can disembuhan if it is still at an early stage. Be aware, clinical breast examination and mammography as a screening procedure is 3 tools to detect cancer early. Need to know, that 9 out of 10 women found a lump in her breast. For primary prevention, it can be done alone. Examination should be done after the menstrual period is completed. Before menstruation, breast slightly swollen making it difficult for the examination. The way the examination is as follows:
A. Stand in front of the mirror and see if there are abnormalities in the breast. Usually these two are not the same breast, the nipple is not located at the same height. Notice if there are wrinkles, grooves, or the nipples are interested. When there is disorder or blood or discharge from the nipple, immediately go to the doctor.
2. Put your arms above your head and look back to the breast.
3. Bend to the breast hanging down, and check again.
4. Lie in bed and put your left hand behind his head, and a pillow under your left shoulder. Touch the left breast with the palm of the right radius. Check if there are lumps in the breast. Then check whether there is a lump or swelling in the left armpit.
5. Check and Touch the nipple and surrounding areas. In general, the mammary glands when touched with your fingers will feel rubbery and easily moved. If there is a tumor, it will feel hard and can not be moved (not to be moved from its place). If you feel there is a lump the size of 1 cm or more, immediately go to the doctor. The earlier treatment, more likely to recover completely. Do the same for breast and right armpit.
TREATMENT OF BREAST CANCER
Before planning a mamma carcinoma therapy, clinical and pathological diagnosis as well as the diffusion rate should be ascertained first. Clinical diagnosis should be similar to the histopathologic diagnosis. If they are different, must be determined which one was wrong. If the purpose curative, it is a consequence of radical action must be done to cure mutilation. But when the follow-surgical palliative actions are useless.
Usually treatment is started after a thorough assessment of the condition of the patient, which is about 1 week or more after the biopsy. Rx consists of surgical and non surgical. Non-surgical therapy consisted of radiation therapy, chemotherapy, hormonal therapy and endocrine. Form of hormone therapy and hormone inhibitors.
Surgery
To get a histological diagnosis of biopsy is usually done so that action can be regarded as the first act in mamma surgery. With frozen preparations, the results can be obtained within 15 minutes. If the examination shows signs of a benign tumor, then the operation is completed, but the results showed a malignant tumor, the operation can proceed with curative surgery.
Surgery is possible curative radical mastectomy, modified radical surgery and conservative surgical excision of the tumor is large.
Always conservative surgery plus axillary lymph node dissection and radiotherapy in the (remaining) breast. Three such measures are a package of treatment that should be implemented simultaneously. In short it is called a therapeutic treatment to preserve the breast.
Curative therapy is performed if the tumor is confined to the breast and there was no infiltration into the chest wall, skin of mamma, or infiltration of the lymph nodes to surrounding structures. If the tumor is called capable agkat with radical surgical follow the entire tumor and its spread in the lymph nodes can be removed. Surgery is done according to the Halstead radical which includes the removal of the breast with most of the skin, m.pektoralis major and minor glands of the armpit and all at once. This is the standard surgical Pemebedahan since the beginning of the 20th century until the '50s.
After the sixties radical surgery is usually performed as modified by Patey. In this operation m. pectoralis major and the minor is maintained if the tumor is free of the obvious mommy muscles.
Curative surgery is now usually done by maintaining the breast. Absolute requirement for this operation is a small tumor and the availability of specific radiotherapy (megavolt) for irradiation. Irradiation is needed to prevent recurrence of the tumor in the breast tumor tissue is left behind or from another tumor nests (multicentric carcinoma).
Thus at the last moment dilakuka usually modified radical surgery (Patey). If it is possible and available means of postoperative irradiation, it is recommended that treatment is a lumpectomy breast maintains extensive axillary lymph node dissection with.
Palliative Surgery in breast cancer is almost never done. Sometimes a solitary residif lokoregional excised, but usually at first have seemed a solitary, but sebenarnnya has spread, so that removal of the tumor is often not useful residif. Amputation is sometimes performed on mamma gland tumor that was not able to lift because of its size and has been estimated by radiotherapy. Although the goal of palliative therapy is sometimes nothing works for quite mean.
Radiotherapy
Radiotherapy in breast cancer is usually used in the curative therapy by maintaining a mamma and as adjunctive therapy or palliative therapy.
Curative radiotherapy as monotherapy lokoregional ineffective, but as an adjunct therapy for curative intent in a relatively large tumor may be useful.
Palliative radiotherapy can be performed with good results for a limited time when the tumor was not able to raise locally. Called tumor could not lift when it reaches the level of T4.
Breast Cancer Radiation Therapy
Radiation therapy is used to kill cancer cells in the removal of the tumor
and the surrounding area, including the lymph nodes (lymph nodes) that can not be resected regional in advanced cancer; in bone metastases, axillary lymph node metastases.
Breast Cancer Chemotherapy
Chemotherapy (a combination of drugs to kill cells that proliferate with
fast or pressing breeding) and drug-hormone inhibitors (drugs that
affect the hormones that promote cancer cell growth) are used to suppress the growth of cancer cells throughout the body. As adjuvant systemic chemotherapy after palliative mastectomy in advanced disease.
Breast Cancer Surgery
Breast cancer surgery called mastectomy. Types of mastectomy:
A. Partial mastectomy (local tumor excision and irradiation). Ranging from lumpectomy to
segmental removal (removal of an extensive network with the affected skin).
2. Total mastectomy with low axial dissection of the entire breast, lymph node dilateral otocpectoralis all minor.
3. Radical mastectomy. The entire breast, pectoralis major and minor muscles underneath: the entire axial.
4. A modified radical mastectomy (Modified Radical Mastectomy).
5. Extended radical mastectomy. Just as radical mastectomy plus internal mammary lymph nodes.
Modified Radical Mastectomy is a surgical oncologist at the malignancy
the breast is to remove the entire breast tissue, all or most of the axial network consisting of stroma and parenkhim entire breast, areola and nipple and the skin over the tumor with axillary lymph node dissection ipsilateral level I, II / III is en bloc without lifting m . pectoralis major and minor.
Indications of operation:
A. Early-stage breast cancer (stage I and II).
2. Locally advanced breast cancer with certain requirements.
3. Soft tissue malignancy of the breast.
Contraindication of operation:
A. Tumor attached to the chest wall.
2. Edema of the arm.
3. Extensive satellite nodules.
4. Inflamatoar mastitis.
Operative action depends on the stage of breast cancer, namely:
A. Breast Cancer Stage I and II
Management of breast cancer stage I and II with radical mastectomy or
modification. Continue with the provision of regional radiation and adjuvant chemotherapy in breast cancer has undergone metastasis. Allegations of metastasis can be determined by examination of the lymph nodes. Simplex mastectomy can we give anyway. Mastectomy should be accompanied by radiation to the tumor bed and regional lymph node regions.
Surgery in T2N1 breast cancer is accompanied by a radical mastectomy radiation
in the local tumor bed and regional lymph nodes. Management of any tumor located in the central or medial quadrant of the breast should be accompanied by radiation in the chain of regional lymph nodes.
Other alternatives can be performed on small tumors Breast conserving therapy techniques. This technique is in the form of a package consisting of removal of the tumor only (tumorektomi) that axillary dissection and radiation with curative (approximately 3 cm tumor size) with certain conditions. How this is done with a wedge excision, segmental resection, partial resection, kwadranektomi, or regular lumpectomy, followed by axillary lymph node dissection in total.
The terms of technique Breast conserving therapy:
A. Primary tumor is not more than 2 cm.
2. N1b is less than 2 cm.
3. There are currently no distant metastasis.
4. No other primary tumor.
5. Contralateral breast cancer free.
6. Breast concerned have never received prior treatment (except lumpectomy).
7. Not performed on small breasts because the cosmetic result is not very prominent.
8. Primary tumor is localized behind the nipple.
2. Stage IIIA Breast Cancer
Management of stage IIIa breast cancer with radical mastectomy, followed
with adjuvant chemotherapy. Simplex or mastectomy followed by radiotherapy to the tumor bed provision and regional lymph nodes.
Modified Radical Mastectomy Technique (Modified Radical Mastectomy)
In brief, the operation technique of modified radical mastectomy (Modified Radical
Mastectomy) can be explained as follows:
A. Patients in general anesthesia, ipsilateral to the operated arm is positioned
900 abduction, shoulder ipsilateral to the operated fouled thin pillow.
2. Disinfection of the operating field, the top until the middle of the neck, the bottom
up to the umbilicus, the contralateral medial to the mid mammma, the
lateral to the lateral edge of the scapula. Disinfected circular upper arm up to
elbow is then wrapped with sterile doek followed by narrowing the field
operation with doek sterile.
3. If found ulcers in breast tumors, the ulcer should be covered with sterile gauze thick (Buick Gaas) and circular stitches.
4. Made an incision (incisional variety is Stewart, Orr, Willy Meyer, Halsted, incisions S) where the line of incision at least within 2 cm from the edge of the tumor, then the flap is created.
5. Flap top to below the clavicle, medially to the parasternal ipsilateral flap, flap down
to the inframammary fold, lateral flap to the anterior edge of m. Latissimus dorsi and identify and vasa. N. Thoracalis dorsalis.
6. Mastectomy starts from the medial to lateral while caring for bleeding, especially branches of blood vessels in the parasternal intercostal. At the time until the lateral edge of m. Haak pectoralis major with the help of mamma tissue removed from the m. Pectoralis minor and serratus anterior (simple mastectomy). In the radical mastectomy pectoral muscle has begun.
7. Axillary dissection begins with finding an enlarged axillary lymph nodes Level I (lateral m.
pectoralis minor), Level II (behind the m. pectoralis minor) and level III (medial m. pectoralis minor). Dissection is not higher in vasa axillary region, because it can lead to edema of the arm. Veins leading to the network mamma ligated. Further identify vasa and n. Thoracalis longus, and thoracalis dorsalis, interkostobrachialis. The next internerural didiseksi KGB and eventually the network regardless mamma and axillary lymph nodes as a single unit (en bloc).
8. The operating field and washed with a solution of Nacl 0.9% sublimat.
9. All the tools are used during surgery was replaced with a new set, as well as
handschoen operator, assistant and instruments as well as doek sterility.
10.Evaluasi re-sources of bleeding.
11.Dipasang 2 pieces drain, large drain (Redon no. 14) is placed below the vasa axillary,
drain is smaller (12) is directed to the medial.
12.Luka lapais closed operation by layer.
Complications of Surgery
Early complications:
A. Bleeding.
2. Lesion n. Thoracalis longus à wing scapula.
3. Lesion n. Thoracalis dorsalis.
Complications Slow
A. Infections.
2. Flap necrosis.
3. Wound dehiscence.
4. Seroma.
5. Edema of the arm.
6. Stiffness of the shoulder joint contractures à.
Palliative actions Breast Cancer
Management is still operabel / kurabel up on stage IIIa. Management
breast cancer stage IIIb and IV is no longer a mastectomy instead of palliative treatment.
Palliative actions aimed at further stages:
A. Maintaining the quality of life of patients in order to keep good / high and regard death
is a normal process.
2. Not accelerate or postpone death.
3. Relieve pain or other complaints are disturbing.
Palliative care is based on the stages, namely:
A. Breast Cancer Stage IIIb
Palliative treatment of breast cancer stage IIIb incisional biopsy and radiation followed.
If the residue does not exist, wait. If relapse, add to the hormonal treatment and chemotherapy. However, when residue remained after radiation, hormonal treatment is given immediately as follows:
In premenopausal patients, bilateral oophorectomy do.
In patients who have 1-5 years of menopause, check the effects of estrogen. If the effect is positive, do it like no. A. If the effect is negative, do it like no. 3. Observation for 6-8 weeks. If a positive response, continue treatment but if the response is negative, do chemotherapy with CMF (CAF) at least 12 cycles for 6 weeks.
In postmenopausal patients, hormonal therapy did inhibitif / additives.
2. Breast Cancer Stage IV
Palliative treatment of stage IV breast cancer, namely:
A. In the premenopausal patients, bilateral oophorectomy do. When a positive response, give or tamofen aminoglutetimid. If relapse or negative response, given CMF chemotherapy (CAF).
2. In patients who have 1-5 years of menopause, check the effects of estrogen. Effects of estrogen can be checked with the estrogen / progesterone receptors (ER / PR). If the effect is positive, do it like no. A. If the effect is negative, do it like no. 31.
3. In the postmenopausal patient, do hormonal therapy, like tamoxifen, estrogen, progesterone, or corticosteroids.
Description: C = cyclophosphamide, M = methotrexate, F = 5-fluourasil.
FOLLOW UP BREAST CANCER
Year 1 and 2 controls every 2 months.
Year 3 s / d 5 control every 3 months.
After 5 years of control every 6 months.
Physical examination: every time control.
Thorax photo: every 6 months.
Lab. Marker: every 2-3 months.
contralateral Mammography: every year or there is any indication.
USG abdomen every 6 months or there is any indication.
Bone scanning: every 2 years or no indication.
APPEAL BREAST CANCER DIAGNOSIS
Differential diagnosis of breast cancer, among others:
A. Mammary fibroadenomas (FAM). Mammary fibroadenoma is a benign breast tumor
commonly found in younger age (15-30 years) with a dense chewy consistency, well defined, painless and cars. Adequate therapy with excision.
2. Fibrocystic disorders. The disorder is benign fibrocystic payudara6 with
solid rubbery consistency / cystic, not demarcated, there is pain, especially before menstruation,
increase in size, usually bilateral / multiple. Medical therapy with symptomatic.
3. Phylodes tumors both malignant and benign, like kistosarkoma filoides. Kistosarkoma filoides resemble mammary fibroadenoma (FAM) are large, oval, well defined, and the car. Can reach 20-30 cm in size. Treatment is with simple mastectomy.
4. Galactocele. Galactocele a cystic tumor mass due to blockage of the channel / lactiferous ducts. These tumors are found on the new mother / nursing.
5. Extensive mastitis. Mastitis is an infection of the breast with a complete inflammatory signs.
Mastitis can develop into an abscess. Mastitis is usually found in women who are breastfeeding. Mastitis is broad, especially in tuberculous mastitis.
6. Other malignancies of the breast (sarcoma, lymphoma, etc.).
CHAPTER IV
CONCLUSION
By looking at the journey of breast neoplasia as the stage through which it can be concluded that early detection of breast cancer can develop methods of breast self examination, clinical breast examination, mammography, ultrasound and computerized tomography. While breast cancer diagnosis can be established by clinical examination, cytology and biopsy.
REFERENCES
1. Fleshman, James W : Schwartz’s Principles of Surgery ed. 7th. New York : Mc. Graw-Hill, 1999.
2. Jong, Wim de & R. Syamsuhidajat : Buku Ajar Ilmu Bedah ed. 2. Jakarta : EGC, 2005.
3. Mansjoer Arif, dkk (Editor). 2000. Bedah Tumor dalam Kapita Selekta Kedokteran. Edisi ke-3, Jilid ke-2. Jakarta : Media Aesculapius Fakultas Kedokteran Universitas Indonesia.
4. Sabiston C. D. Jr, MD., 1997, dalam Buku Ajar Bedah 2, EGC, Jakarta
5. Anonymous. 2007. Kanker Payudara. http://www.blogdokter.net/2007/03/13/kanker-payudara/. 12 Januari 2009.
6. Harnawati AJ. 2008. Askep Kanker Payudara. http://harnawatiaj.wordpress.com/2008/04/16/askep-kanker-payudara/. 29 Desember 2008.
7. Anonymous. 2008. Mastektomi Radikal Modifikasi (MRM). http://bedahumum.wordpress.com/ category/bedah-tumor/. 12 Januari 2009
8. http://ajangberkarya.wordpress.com/2008/07/26/karsinoma-kanker-payudara/
9. http://medlinux.blogspot.com/2009/03/karsinoma-payudara.html
2. Jong, Wim de & R. Syamsuhidajat : Buku Ajar Ilmu Bedah ed. 2. Jakarta : EGC, 2005.
3. Mansjoer Arif, dkk (Editor). 2000. Bedah Tumor dalam Kapita Selekta Kedokteran. Edisi ke-3, Jilid ke-2. Jakarta : Media Aesculapius Fakultas Kedokteran Universitas Indonesia.
4. Sabiston C. D. Jr, MD., 1997, dalam Buku Ajar Bedah 2, EGC, Jakarta
5. Anonymous. 2007. Kanker Payudara. http://www.blogdokter.net/2007/03/13/kanker-payudara/. 12 Januari 2009.
6. Harnawati AJ. 2008. Askep Kanker Payudara. http://harnawatiaj.wordpress.com/2008/04/16/askep-kanker-payudara/. 29 Desember 2008.
7. Anonymous. 2008. Mastektomi Radikal Modifikasi (MRM). http://bedahumum.wordpress.com/ category/bedah-tumor/. 12 Januari 2009
8. http://ajangberkarya.wordpress.com/2008/07/26/karsinoma-kanker-payudara/
9. http://medlinux.blogspot.com/2009/03/karsinoma-payudara.html
1. Fleshman, James W : Schwartz’s Principles of Surgery ed. 7th. New York : Mc. Graw-Hill, 1999.
2. Jong, Wim de & R. Syamsuhidajat : Buku Ajar Ilmu Bedah ed. 2. Jakarta : EGC, 2005.
3. Mansjoer Arif, dkk (Editor). 2000. Bedah Tumor dalam Kapita Selekta Kedokteran. Edisi ke-3, Jilid ke-2. Jakarta : Media Aesculapius Fakultas Kedokteran Universitas Indonesia.
4. Sabiston C. D. Jr, MD., 1997, dalam Buku Ajar Bedah 2, EGC, Jakarta
5. Anonymous. 2007. Kanker Payudara. http://www.blogdokter.net/2007/03/13/kanker-payudara/. 12 Januari 2009.
6. Harnawati AJ. 2008. Askep Kanker Payudara. http://harnawatiaj.wordpress.com/2008/04/16/askep-kanker-payudara/. 29 Desember 2008.
7. Anonymous. 2008. Mastektomi Radikal Modifikasi (MRM). http://bedahumum.wordpress.com/ category/bedah-tumor/. 12 Januari 2009
8. http://ajangberkarya.wordpress.com/2008/07/26/karsinoma-kanker-payudara/
9. http://medlinux.blogspot.com/2009/03/karsinoma-payudara.html
2. Jong, Wim de & R. Syamsuhidajat : Buku Ajar Ilmu Bedah ed. 2. Jakarta : EGC, 2005.
3. Mansjoer Arif, dkk (Editor). 2000. Bedah Tumor dalam Kapita Selekta Kedokteran. Edisi ke-3, Jilid ke-2. Jakarta : Media Aesculapius Fakultas Kedokteran Universitas Indonesia.
4. Sabiston C. D. Jr, MD., 1997, dalam Buku Ajar Bedah 2, EGC, Jakarta
5. Anonymous. 2007. Kanker Payudara. http://www.blogdokter.net/2007/03/13/kanker-payudara/. 12 Januari 2009.
6. Harnawati AJ. 2008. Askep Kanker Payudara. http://harnawatiaj.wordpress.com/2008/04/16/askep-kanker-payudara/. 29 Desember 2008.
7. Anonymous. 2008. Mastektomi Radikal Modifikasi (MRM). http://bedahumum.wordpress.com/ category/bedah-tumor/. 12 Januari 2009
8. http://ajangberkarya.wordpress.com/2008/07/26/karsinoma-kanker-payudara/
9. http://medlinux.blogspot.com/2009/03/karsinoma-payudara.html
No comments:
Post a Comment